What Is Apicoectomy Surgery and How Does It Relate to Endodontics?
Apicoectomy surgery is a specialized endodontic procedure that involves removing the tip of a tooth’s root along with surrounding infected tissue. This microsurgical technique falls under the broader field of endodontics, which focuses on treating the interior structures of teeth, particularly the pulp and root canal system.
When conventional root canal treatment fails to resolve persistent infection or inflammation at the root apex, an apicoectomy becomes necessary. The procedure directly addresses issues that cannot be reached through standard canal treatment, making it an essential component of advanced endodontic care aimed at preserving natural teeth.
Why Is Apicoectomy Surgery Considered a Microsurgical Endodontic Procedure?
Apicoectomy is classified as microsurgical because it requires extremely precise techniques and specialized equipment, including surgical microscopes and ultrasonic instruments. The procedure involves working in a very small area typically just 3 millimeters of the root tip demanding exceptional accuracy and visualization.
Endodontists use high-powered magnification to identify tiny canals, cracks, and infected tissue that would be invisible to the naked eye. This microsurgical approach significantly improves success rates compared to traditional methods, with modern techniques achieving success rates of 85-95%. The minimally invasive nature also results in faster healing, less discomfort, and better preservation of surrounding bone and tissue structures.
How Does Apicoectomy Differ From a Standard Root Canal Treatment?
Standard root canal treatment accesses the tooth’s interior from the crown, working down through the canal system to remove infected pulp and bacteria. Apicoectomy takes the opposite approach, accessing the root tip surgically from outside the tooth through the gum and bone. Root canal therapy is typically the first-line treatment for infected teeth, performed through the existing tooth structure without requiring incisions.
Apicoectomy, however, is a surgical procedure requiring local anesthesia, incisions in the gum tissue, and temporary bone removal. While root canal treatment addresses infections within the canal system, apicoectomy specifically targets persistent infections at the root apex that cannot be resolved through conventional endodontic approaches.
What Happens When Root Canal Therapy Fails?
Root canal failure occurs when bacteria persist or reinfect the treated tooth, causing continued inflammation or infection around the root apex. This can happen due to complex canal anatomy, missed accessory canals, inadequate cleaning, bacterial regrowth, or new infection introduced during crown placement.
Symptoms of failure include persistent pain, swelling, abscess formation, or bone loss visible on X-rays. The infection can create periapical lesions pockets of infected tissue at the root tip that won’t heal despite initial treatment. In these cases, retreatment through the crown may be attempted first, but when that’s not feasible due to posts, crowns, or anatomical complications, apicoectomy becomes the necessary intervention to save the tooth.
Why Is Apicoectomy the Last Step Before Tooth Extraction?
Apicoectomy represents the final conservative treatment option for saving a tooth that hasn’t responded to conventional endodontic therapy. After this procedure, there are limited additional interventions available if infection persists, making extraction the next logical step. The procedure physically removes the infected root apex and seals the remaining root end, addressing issues that cannot be resolved any other way without removing the entire tooth.
Dentists prefer exhausting all tooth-saving options before extraction because preserving natural teeth maintains better oral function, prevents bone loss, and avoids the need for prosthetic replacements. However, if apicoectomy fails or isn’t technically feasible, extraction becomes necessary to eliminate infection and protect overall oral health.
When Is Apicoectomy Surgery Needed?
Apicoectomy surgery becomes necessary when persistent infection or inflammation exists at the root tip of a tooth despite previous root canal treatment. This procedure is indicated when conventional retreatment isn’t possible or has already failed, when there are anatomical complications preventing access through the crown, or when a lesion at the root apex won’t heal.
Common scenarios include teeth with posts or crowns that make retreatment impractical, roots with complex anatomy or calcification, separated instruments blocking the canal, or perforations in the root. The surgery may also be needed to investigate suspected root fractures or remove foreign materials. Essentially, apicoectomy is required when saving the tooth demands direct surgical access to the root tip.
What Symptoms Indicate That a Tooth May Require Apicoectomy?
Symptoms suggesting the need for apicoectomy include persistent pain or sensitivity in a previously root canal-treated tooth, especially when biting or applying pressure. Patients may experience recurring gum swelling, pimple-like bumps on the gums (fistulas) that drain pus, or tenderness in the area around the tooth root.
Some individuals notice prolonged sensitivity to hot or cold temperatures, even months after initial treatment. Visible signs include gum discoloration or swelling near the affected tooth. However, many cases are asymptomatic, discovered only through routine X-rays showing bone loss or dark shadows at the root apex. Chronic bad taste or odor from persistent infection may also occur, prompting investigation and potential surgical intervention.
How Do Dentists Diagnose the Need for Apicoectomy in Turkey?
Turkish dentists diagnose the need for apicoectomy through comprehensive clinical examination combined with advanced imaging technology. The process begins with reviewing the patient’s dental history, symptoms, and previous treatments. Dentists perform visual inspection and palpation tests to assess swelling, tenderness, or abnormalities. Percussion and bite tests help identify specific problematic teeth.
Thermal sensitivity tests may be conducted to evaluate nerve vitality. However, the most critical diagnostic tools are radiographic images that reveal bone loss, periapical lesions, or other pathology around the root apex. Turkish dental clinics typically utilize both traditional X-rays and cutting-edge 3D imaging to create comprehensive treatment plans before recommending apicoectomy surgery.
What Role Do Digital X-rays and 3D Scans Play in Diagnosis?
Digital X-rays and 3D cone beam computed tomography (CBCT) scans are essential for accurately diagnosing the need for apicoectomy and planning the procedure. Digital X-rays provide two-dimensional images showing bone loss, lesion size, and root anatomy with significantly less radiation exposure than traditional films.
CBCT scans offer three-dimensional visualization, revealing the exact position of the root apex, proximity to anatomical structures like sinuses or nerves, and the extent of bone involvement. These advanced imaging techniques help endodontists identify hidden canals, root fractures, or perforations that might not be visible on standard X-rays. The detailed information allows for precise surgical planning, improving success rates and minimizing complications during the apicoectomy procedure.
How Is Apicoectomy Surgery Performed Step by Step?
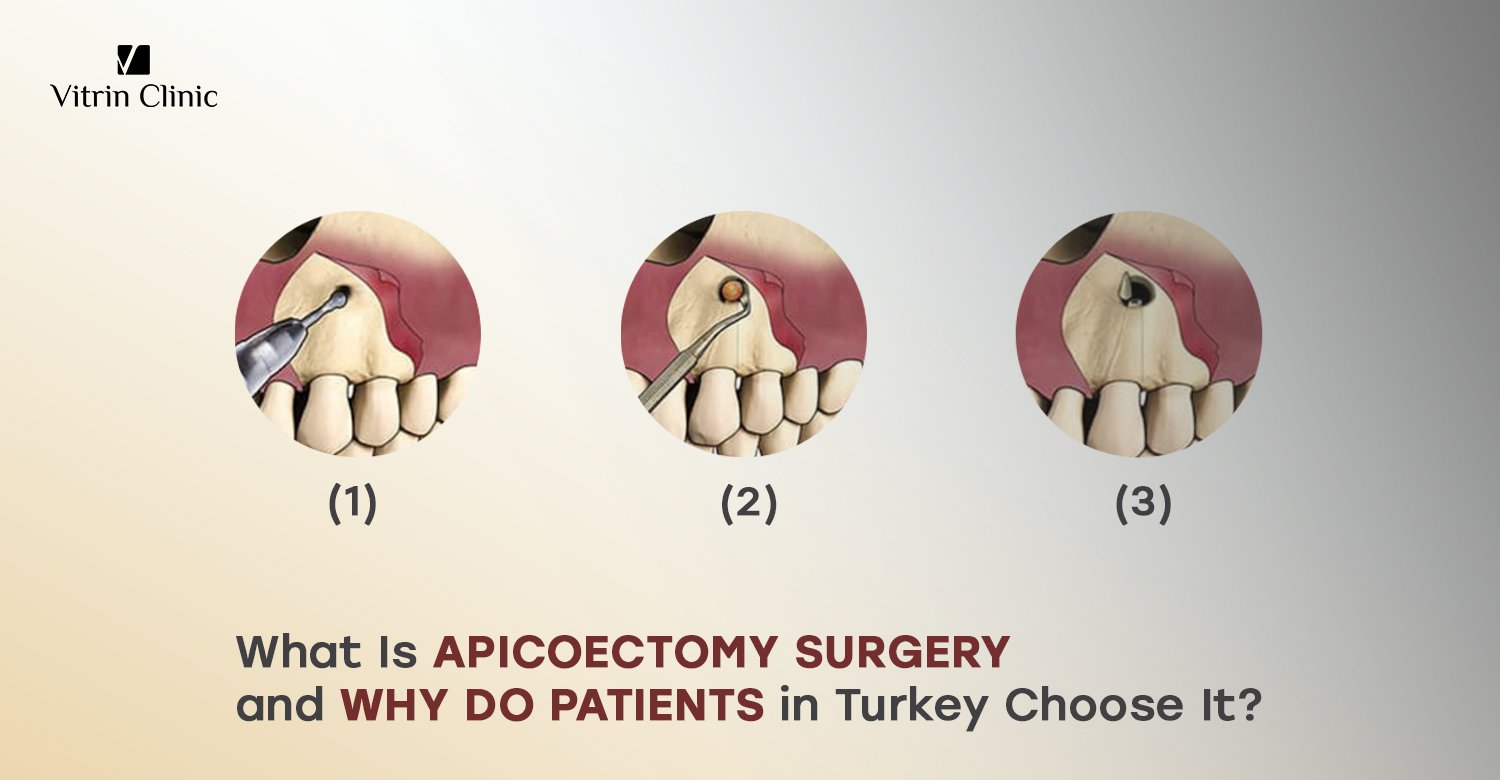
Apicoectomy surgery follows a systematic approach beginning with local anesthesia administration to ensure patient comfort. The surgeon makes a small incision in the gum tissue near the affected tooth root, then carefully folds back the gum to expose the underlying bone.
Using specialized instruments or ultrasonic devices, a small window is created in the bone to access the root tip. The infected root apex is then removed (typically 3mm), along with surrounding infected tissue and any cysts or granulomas. The root end is cleaned and prepared, then sealed with biocompatible filling material. Finally, the gum tissue is repositioned and sutured. The entire procedure typically takes 30-90 minutes depending on tooth location and complexity.
What Preparation Steps Are Taken Before the Surgery?
Before apicoectomy surgery, patients undergo thorough evaluation including medical history review to identify allergies, medications, or health conditions affecting treatment. Comprehensive imaging studies are analyzed to plan the surgical approach. Patients receive detailed pre-operative instructions, which may include fasting guidelines if sedation is planned, arranging transportation home, and discontinuing certain medications like blood thinners if medically appropriate.
Antibiotics might be prescribed preventively in some cases. On the day of surgery, the surgical site is cleaned and sterilized. The patient is positioned comfortably, and monitoring equipment may be attached. Local anesthesia is administered and allowed adequate time to take full effect before any incision is made, ensuring complete numbness throughout the procedure.
How Does the Surgeon Access the Tooth Root Tip?
The surgeon accesses the tooth root tip through a carefully designed gum incision that provides optimal visibility while minimizing tissue trauma. After achieving adequate anesthesia, a full-thickness mucoperiosteal flap is created by making an incision in the gum tissue, typically extending from one tooth beyond the affected area to ensure sufficient access.
The gum and underlying periosteum are gently reflected away from the bone using specialized elevators. Once the bone covering the root tip is exposed, the surgeon uses a surgical handpiece or ultrasonic instrument to create a small window in the cortical bone, carefully removing enough bone to visualize the root apex and surrounding infected tissue. This access window is precisely positioned using pre-surgical imaging as a guide.
What Is Root-End Resection and Why Is It Important?
Root-end resection is the process of removing approximately 3 millimeters from the tip of the tooth root along with any infected or damaged tissue surrounding it. This step is critically important because it eliminates the portion of the root where infection persists, including complex canal anatomy, lateral canals, and isthmuses that cannot be adequately cleaned through conventional root canal treatment.
The resection creates a fresh, clean surface that can be properly sealed. By removing the infected apex, the procedure eliminates the source of continued inflammation and bone destruction. The angled cut (typically perpendicular to the root axis) also exposes the canal system for direct visualization, allowing the surgeon to identify and address any issues contributing to treatment failure.
How Is the Infected Tissue Removed Safely?
Infected tissue removal during apicoectomy requires meticulous surgical technique to eliminate all pathological material while preserving healthy structures. After resecting the root tip, the surgeon uses curettes and surgical instruments to carefully debride the bony cavity, removing granulation tissue, cysts, or abscesses surrounding the root apex.
The area is thoroughly irrigated with sterile saline solution to flush out debris and bacteria. Hemostasis (bleeding control) is achieved using pressure, hemostatic agents, or electrocautery as needed. The surgeon works under magnification to ensure complete removal of infected tissue while avoiding damage to adjacent teeth roots, nerves, blood vessels, or vital anatomical structures. All removed tissue is typically sent for histopathological examination to rule out unexpected pathology.
What Materials Are Used to Seal the Root Canal End?
Modern apicoectomy procedures primarily use mineral trioxide aggregate (MTA) or similar biocompatible materials to seal the root canal end. MTA is the gold standard because it provides excellent sealing properties, promotes healing, is biocompatible with surrounding tissues, and can set even in the presence of moisture. Alternative materials include Super-EBA, IRM (intermediate restorative material), or newer bioceramic sealers.
The chosen material is carefully placed into a small preparation made in the resected root end using ultrasonic tips, creating a retrograde filling that seals the canal system from the apex. This seal prevents bacteria from exiting the canal system into surrounding bone tissue, which is essential for healing and long-term success of the apicoectomy procedure.
How Long Does Apicoectomy Surgery Usually Take?
Apicoectomy surgery typically takes between 30 to 90 minutes to complete, though duration varies based on several factors. Front teeth (incisors and canines) generally require 30-45 minutes due to easier access and simpler root anatomy. Premolars typically take 45-60 minutes, while molars, especially upper molars near the sinus cavity may require 60-90 minutes due to difficult access, multiple roots, and complex anatomy.
Additional time is needed if treating multiple roots simultaneously or addressing complicated lesions. The surgeon’s experience, use of surgical microscopes, and any unexpected findings during surgery also influence procedure length. Despite this time investment, the microsurgical precision ensures optimal outcomes. Patients should plan for approximately 2-3 hours at the clinic including preparation and immediate post-operative care.
What Kind of Anesthesia Is Used During Apicoectomy?
Apicoectomy is typically performed under local anesthesia, which completely numbs the surgical area while the patient remains fully conscious and able to communicate. The endodontist injects local anesthetic solution (usually antiacne or lidocaine with epinephrine) near the tooth and surrounding tissues, ensuring profound numbness before beginning.
For anxious patients or complex cases, conscious sedation options may be offered, including oral sedation medications taken before the procedure or nitrous oxide (laughing gas) administered during treatment. These sedation methods help patients relax while local anesthesia handles pain control. In rare cases requiring treatment of multiple teeth or for patients with severe dental anxiety, IV sedation performed by an anesthesiologist might be arranged. General anesthesia is extremely uncommon for apicoectomy and reserved for special circumstances.
What Are the Benefits of Apicoectomy Surgery?
Apicoectomy surgery offers significant benefits, primarily preserving natural teeth that would otherwise require extraction. This procedure successfully resolves persistent infections that don’t respond to conventional treatment, preventing the spread of bacteria to adjacent teeth and surrounding bone structures. By eliminating infected tissue and sealing the root apex, apicoectomy stops ongoing bone destruction and allows for regeneration of healthy bone tissue.
The procedure maintains natural bite function, prevents shifting of adjacent teeth, and preserves the jawbone structure that would deteriorate after tooth loss. From an economic perspective, saving the natural tooth is more cost-effective long-term than extraction followed by implant placement. Additionally, apicoectomy avoids the psychological impact of tooth loss and eliminates the need for prosthetic replacement options.
How Does Apicoectomy Help Save Natural Teeth?
Apicoectomy helps save natural teeth by providing a final opportunity to eliminate persistent infection when all other conservative treatments have failed. The procedure surgically removes the infected root apex and surrounding pathological tissue, addressing problems that cannot be reached through conventional root canal retreatment. By directly accessing and sealing the root end, apicoectomy eliminates bacterial reservoirs hiding in complex anatomical structures like lateral canals, isthmuses, and apical deltas.
This targeted approach resolves the underlying infection while preserving the remaining healthy tooth structure and supporting tissues. Without apicoectomy, teeth with persistent apical infections would require extraction, leading to bone loss, tooth migration, bite problems, and the need for expensive replacements like implants or bridges. The procedure effectively extends tooth lifespan for many years.
Can Apicoectomy Prevent the Spread of Dental Infections?
Apicoectomy effectively prevents the spread of dental infections by eliminating the source of bacteria at the root apex and creating a hermetic seal. Untreated periapical infections can spread through bone and soft tissues, potentially causing serious complications including cellulitis, Ludwig’s angina, or even life-threatening systemic infections. The bacteria from an infected root tip can also travel to adjacent teeth, compromising their health and viability.
By surgically removing infected tissue and properly sealing the root canal system, apicoectomy stops bacterial proliferation and prevents further contamination. The procedure also promotes healing and bone regeneration around the treated area, restoring healthy tissue barriers. This containment and elimination of infection protects overall oral health and prevents systemic complications associated with chronic dental infections.
How Does Apicoectomy Improve Oral Health in the Long Term?
Apicoectomy improves long-term oral health by resolving chronic infections that would otherwise continuously compromise the immune system and oral tissues. Successfully treated teeth continue functioning normally for many years, maintaining proper occlusion and preventing the cascade of problems following tooth loss. The procedure stops ongoing bone destruction, allowing for regeneration and preservation of alveolar ridge height, which is crucial for facial structure and future dental work.
By saving natural teeth, apicoectomy prevents adjacent teeth from shifting or tilting, which can cause bite problems, TMJ issues, and increased cavity risk. The procedure eliminates chronic inflammation that may contribute to systemic health issues. Maintaining natural dentition also supports better nutrition through improved chewing function and preserves psychological well-being associated with having complete, natural dentition.
What Are the Risks and Complications of Apicoectomy Surgery?
Apicoectomy surgery, while generally safe and successful, carries potential risks and complications like any surgical procedure. Common minor issues include temporary swelling, bruising, discomfort, and bleeding at the surgical site. More significant but less frequent complications include nerve damage causing temporary or rarely permanent numbness or tingling in the lip, chin, or tongue, particularly with lower teeth. Infection may develop post-operatively despite prophylactic measures.
Sinus complications can occur when treating upper back teeth, potentially creating an oral-sinus communication. Root damage, perforation, or fracture may happen during the procedure. Adjacent tooth damage is possible though rare. Some patients experience prolonged healing or incomplete bone regeneration. The procedure itself may fail to resolve infection, requiring extraction. Proper surgical technique, thorough pre-operative planning, and experienced practitioners significantly minimize these risks.
What Are the Most Common Side Effects After Surgery?
The most common side effects following apicoectomy include swelling of the gum tissues and face adjacent to the surgical site, typically peaking 48-72 hours post-surgery before gradually subsiding. Bruising may appear, sometimes extending to the cheek or under the jaw, displaying yellow, purple, or green discoloration that resolves within 7-10 days. Moderate pain or discomfort is expected, usually managed effectively with prescribed or over-the-counter pain medications.
Mild bleeding or oozing from the incision site is normal for the first 24 hours. Temporary tooth sensitivity to pressure or temperature changes may occur. Many patients report feeling tired the day of surgery. Jaw stiffness or difficulty opening the mouth fully can persist for several days. Some numbness or tingling near the surgical area is common initially and typically resolves within weeks.
How Often Do Apicoectomy Surgeries Fail?
Apicoectomy surgeries have a success rate of 85-95% when performed using modern microsurgical techniques, meaning failure occurs in approximately 5-15% of cases. Failure rates vary depending on multiple factors including tooth location, complexity of root anatomy, quality of root canal filling, presence of root fractures, and patient health status.
Front teeth generally have higher success rates (90-95%) compared to molars (80-90%) due to easier access and simpler anatomy. When performed by experienced endodontists using surgical microscopes and contemporary materials like MTA, success rates approach the higher end of this range. Failure typically manifests as persistent symptoms, continued bone loss on X-rays, or recurring infection within months to a few years post-surgery. Failed apicoectomies generally require tooth extraction as no further conservative treatment options remain available.
What Factors Can Affect the Success Rate of Apicoectomy?
Multiple factors influence apicoectomy success rates, including the quality of the root canal treatment preceding the surgery, inadequate canal obturation significantly reduces success. Tooth-specific factors include presence of vertical root fractures (which contraindicate apicoectomy), tooth location (anterior teeth have better prognoses than posterior), and root anatomy complexity.
The size of the periapical lesion matters, with larger lesions having slightly lower success rates. Surgical technique factors include using magnification, proper root-end preparation, and quality sealing materials like MTA. Patient-related factors encompass overall health status, immune system function, smoking habits, diabetes control, and compliance with post-operative instructions. The surgeon’s experience and skill level significantly impact outcomes. Proper case selection is crucial attempting apicoectomy on teeth with poor long-term prognoses reduces overall success statistics without benefiting patients.
How Do Gum Health and Bone Quality Influence Success?
Gum health and bone quality are critical factors determining apicoectomy success. Healthy gingival tissues provide proper blood supply essential for healing, while periodontal disease compromises the supporting structures and increases infection risk. Patients with good periodontal health experience faster healing, better tissue regeneration, and reduced post-operative complications. Bone quality significantly affects surgical access, stability of adjacent structures, and regenerative capacity.
Dense, healthy bone provides excellent support and predictably regenerates after surgery, completely filling the defect created by infection and surgical intervention. Poor bone quality whether from osteoporosis, previous infections, or systemic conditions may result in incomplete healing, inadequate bone fill, or persistent lesions. The bone’s vascular supply directly influences infection resistance and healing speed. Pre-existing bone loss or compromised bone health should be carefully evaluated when determining apicoectomy feasibility.
Can Smoking or Health Conditions Affect Healing?
Smoking significantly impairs healing after apicoectomy surgery by reducing blood flow to tissues, decreasing oxygen delivery, impairing immune function, and introducing harmful chemicals that interfere with tissue repair. Smokers experience higher complication rates, including increased infection risk, delayed healing, and reduced success rates compared to non-smokers. Ideally, patients should stop smoking at least two weeks before and throughout the healing period.
Systemic health conditions also substantially impact outcomes uncontrolled diabetes impairs wound healing and increases infection susceptibility. Immunocompromised patients from HIV, chemotherapy, or immunosuppressive medications face higher failure risks.
Osteoporosis or bisphosphonate use may affect bone healing. Blood disorders affecting clotting require special management. Patients should disclose all medical conditions and medications during consultation. Some conditions may necessitate treatment optimization before surgery or may even contraindicate the procedure entirely.
What Is Recovery Like After Apicoectomy Surgery?
Recovery after apicoectomy surgery typically progresses through several predictable phases. The first 24-48 hours involve the most discomfort, with swelling, mild pain, and possible minor bleeding. Peak swelling usually occurs around day 2-3, then gradually decreases. Most patients can return to work or normal activities within 2-3 days, though complete soft tissue healing takes 1-2 weeks. Sutures are typically removed after 5-7 days if non-dissolvable.
The underlying bone requires several months to completely regenerate, though patients won’t notice this process. Initial radiographic healing signs appear within 3-6 months, with complete bone fill sometimes taking up to one year. During recovery, patients should follow prescribed medications, maintain gentle oral hygiene, eat soft foods, and attend follow-up appointments to monitor healing progress and ensure successful outcomes.
How Long Does It Take to Heal After Apicoectomy?
Healing after apicoectomy occurs in stages with varying timeframes. Superficial soft tissue healing of the incision site takes approximately 7-10 days, after which sutures are removed and the gum appears relatively normal. However, complete gum tissue maturation continues for several weeks. Patients typically feel back to normal within 2 weeks, though some residual tenderness may persist for 3-4 weeks. و
The crucial bone healing process takes considerably longer initial bone formation begins within weeks, but radiographic evidence of healing appears at 3-6 month follow-up appointments. Complete bone regeneration and remodeling can take 6-12 months, occasionally longer for large lesions. The tooth itself stabilizes within weeks, though it may feel slightly different for several months. Overall success is typically evaluated at the one-year follow-up appointment through clinical examination and radiographic assessment showing complete bone fill.
What Pain Management Options Are Recommended?
Pain management after apicoectomy begins with ice application during the first 24 hours15 minutes on, 15 minutes off to reduce swelling and provide numbing relief. Over-the-counter medications like ibuprofen (400-600mg every 6-8 hours) effectively manage most post-operative discomfort while reducing inflammation. Some patients combine ibuprofen with acetaminophen for enhanced pain control.
For moderate to severe pain, dentists may prescribe stronger medications like codeine combinations or tramadol for short-term use. Prescription NSAIDs like ketorolac might be provided. Most patients find pain peaks within the first 48 hours, then rapidly improves. Keeping the head elevated, even while sleeping, helps minimize swelling and associated discomfort. Patients should take pain medications as directed rather than waiting for pain to become severe. Persistent or worsening pain beyond expected timeframes requires immediate dental evaluation.
What Post-Surgery Care Instructions Should Patients Follow?
Post-surgery care instructions are crucial for optimal healing. Patients should bite on gauze for 30 minutes immediately after surgery to control bleeding, avoiding vigorous rinsing or spitting for 24 hours. Ice packs applied externally help reduce swelling during the first day. Take all prescribed medications as directed, including antibiotics if prescribed.
Maintain gentle oral hygiene carefully brush teeth avoiding the surgical site initially, then gently clean the area after 24 hours. Rinse with warm salt water (1 teaspoon salt in 8 oz water) starting the day after surgery, 3-4 times daily. Avoid strenuous exercise, heavy lifting, or bending over for 3-5 days. Don’t smoke or use straws, as suction can dislodge clots. Sleep with head elevated on extra pillows. Attend all scheduled follow-up appointments for suture removal and healing assessment.
What Foods Should Be Avoided After Apicoectomy?
After apicoectomy, patients should avoid hard, crunchy, chewy, or sharp foods that could traumatize the surgical site or dislodge sutures. Specifically avoid nuts, chips, popcorn, hard bread, raw vegetables, tough meats, sticky candies, and anything requiring vigorous chewing. Very hot foods and beverages should be avoided for the first few days as they can increase bleeding and discomfort.
Acidic foods like citrus fruits or tomato sauce may irritate the healing tissue. Spicy foods can cause discomfort. Avoid alcohol while taking pain medications and for the first week as it impairs healing. Don’t use straws or smoke, as suction can dislodge blood clots. Instead, consume soft foods like yogurt, smoothies, mashed potatoes, soups (lukewarm), scrambled eggs, pasta, ice cream, and protein shakes. Gradually reintroduce normal foods as comfort allows, typically within 7-10 days.
How Important Is Oral Hygiene During Recovery?
Oral hygiene during apicoectomy recovery is critically important for preventing infection and promoting optimal healing, though it requires modification from normal routines. Good oral hygiene removes bacteria and food debris that could infect the surgical site while promoting healthy tissue regeneration. However, patients must be gentle around the operated area to avoid disrupting sutures or the healing gum tissue.
After 24 hours, patients should carefully brush all teeth, avoiding direct contact with the incision line initially. Gentle rinsing with warm salt water 3-4 times daily helps keep the area clean and promotes healing. By day 3-5, patients can gently clean the surgical area with a soft toothbrush. Prescribed antimicrobial rinses should be used as directed. Proper hygiene prevents bacterial accumulation that could compromise healing or cause infection, ultimately determining surgery success.
How Much Does Apicoectomy Surgery Cost in Turkey?
Apicoectomy surgery in Turkey typically costs between $200-400 per tooth, representing a fraction of prices in Western countries. This cost usually includes the surgical procedure, local anesthesia, medications, follow-up appointments, and often diagnostic imaging. The price varies depending on tooth location (front teeth less expensive than molars), complexity of the case, clinic location and reputation, and the dentist’s experience and credentials.
Some clinics offer package deals for international patients including airport transfers, accommodation assistance, and translation services. Despite the significantly lower costs, Turkish dental clinics maintain high standards using modern equipment and materials comparable to Western facilities. Many dentists hold international certifications and speak English fluently. The affordability combined with quality care makes Turkey increasingly popular for dental tourism, particularly for procedures like apicoectomy.
Why Is Apicoectomy Surgery More Affordable in Turkey?
Apicoectomy surgery is more affordable in Turkey primarily due to lower operational costs, including significantly cheaper rent for clinic spaces, reduced staff salaries, and lower overhead expenses compared to Western countries. The favorable exchange rate of the Turkish Lira against major currencies like dollars and euros makes prices appear even more competitive for international patients. Turkey’s lower cost of living means dentists can charge less while maintaining comfortable incomes.
Additionally, Turkey has invested heavily in dental education and medical tourism infrastructure, creating competitive market conditions that keep prices reasonable while maintaining quality. There are no compromises in treatment standards Turkish dentists use the same materials (MTA, bio ceramics), equipment (surgical microscopes), and techniques as Western practitioners. Government support for medical tourism and streamlined regulatory processes also contribute to cost efficiency passed onto patients.
What Factors Influence the Cost of Apicoectomy?
Several factors influence apicoectomy costs in Turkey. Tooth location significantly affects price front teeth (incisors, canines) are generally least expensive at $200-300, premolars are mid-range at $250-350, while molars cost $300-400 due to difficult access and complex anatomy. Case complexity matters straightforward cases cost less than those involving large lesions, multiple canals, or anatomical complications.
The dentist’s qualifications and experience level impact pricing, with specialized endodontists or those with advanced certifications charging premium rates. Clinic location and facility quality factor in modern clinics in major cities like Istanbul or Antalya may charge more than facilities in smaller cities. Technology use including surgical microscopes and 3D imaging may increase costs. Additional procedures like bone grafting or treatment of multiple roots simultaneously also raise the total price.
Does Location Within Turkey Affect the Price?
Location within Turkey significantly affects apicoectomy pricing. Major metropolitan areas like Istanbul, Ankara, and Izmir generally have higher costs due to elevated operating expenses including rent, utilities, and staff salaries. Tourist-destination cities like Antalya also command premium prices due to high international patient volumes and developed medical tourism infrastructure. Clinics in upscale neighborhoods or popular districts charge more than those in less central areas.
However, competition in major cities can sometimes drive prices down. Smaller cities and towns typically offer lower prices sometimes 20-30% less than Istanbul though they may have fewer English-speaking dentists or specialized endodontists. The quality difference isn’t necessarily proportional to price variation; excellent care exists throughout Turkey. International patients often choose major cities despite higher costs for convenience, English proficiency, and established medical tourism services.
How Does the Dentist’s Experience Impact Cost?
The dentist’s experience and credentials substantially impact apicoectomy costs. Endodontists specialists with additional years of training specifically in root canal procedures and surgeries typically charge 20-40% more than general dentists performing the same procedure. Highly experienced practitioners with 15+ years of performing apicoectomies command premium rates justified by superior success rates and fewer complications. Dentists with international certifications, fellowships, or memberships in prestigious organizations may charge more.
Those regularly attending continuing education courses and using latest techniques and technologies often price services higher. Practitioners with established reputations, published research, or teaching positions at universities typically have premium pricing. However, higher cost doesn’t always guarantee better outcomes many mid-career dentists offer excellent results at moderate prices. Patients should consider credentials, before-after cases, patient reviews, and success rate statistics alongside cost when selecting a provider.
How Does the Cost in Turkey Compare to Europe and the US?
Apicoectomy costs in Turkey are dramatically lower compared to Europe and the United States. In the US, the procedure typically costs $1,000-2,000 per tooth, sometimes exceeding $2,500 in major metropolitan areas or with specialist endodontists. Western European countries like the UK, Germany, or Switzerland charge €800-1,800 ($900-2,000) per tooth.
Even Eastern European countries like Poland or Hungary, popular for dental tourism, charge €400-700 ($450-800). Turkey’s $200-400 range represents savings of 60-85% compared to Western prices. For patients needing treatment on multiple teeth, savings become substantialpotentially $3,000-5,000 or more. When factoring in that many international patients combine dental treatment with tourism, the value proposition strengthens. Even including flight costs and accommodation, patients typically save 50-70% overall while receiving comparable or superior care using identical materials and techniques.
Who Are the Best Candidates for Apicoectomy Surgery?
The best candidates for apicoectomy are adults with specific clinical conditions: teeth with persistent periapical infections despite proper root canal treatment, teeth that cannot be retreated conventionally due to posts, crowns, or calcified canals, and patients wanting to preserve natural teeth rather than opt for extraction. Ideal candidates have good general health, adequate bone support around the affected tooth, and absence of significant periodontal disease.
The tooth should have sufficient remaining structure to function long-term post-surgery. Patients must be able to tolerate minor oral surgery with local anesthesia and commit to proper post-operative care. Motivated patients who understand the procedure, maintain good oral hygiene, and attend follow-up appointments achieve best outcomes. Non-smokers or those willing to quit temporarily have better success rates. Patients without contraindications like uncontrolled systemic diseases or bleeding disorders are ideal candidates.
Can Children or Teenagers Undergo Apicoectomy?
Children and teenagers can undergo apicoectomy, though it’s relatively uncommon as this age group typically hasn’t had extensive dental work or root canal failures. The procedure is considered when young patients have traumatic injuries causing root damage, previous pulp therapy complications, or developmental abnormalities affecting root formation. In growing patients, dentists carefully evaluate whether tooth development is complete, as operating on immature roots presents challenges.
The timing must consider ongoing jaw and facial growth. Young patients generally heal faster than adults due to superior regenerative capacity. However, considerations include their ability to tolerate the procedure, cooperate with post-operative instructions, and maintain adequate oral hygiene during healing. Pediatric endodontists or those experienced treating children should perform the procedure. The psychological aspect matters ensuring the child understands and isn’t traumatized by surgical intervention is crucial.
Is Apicoectomy Suitable for Patients With Dental Implants?
Apicoectomy can be suitable for patients who already have dental implants, though special considerations apply. The procedure itself doesn’t affect existing implants in other areas of the mouth. However, if an apicoectomy is needed on a tooth adjacent to an implant, careful surgical planning is essential to avoid damaging the implant or surrounding bone. The proximity of roots to implants must be evaluated through 3D imaging to ensure adequate space for surgical access.
Patients considering future implants might choose apicoectomy to save their natural tooth, avoiding implant placement altogether. If apicoectomy fails, subsequent implant placement is still possible, though bone grafting may be needed if significant bone loss occurred. Some patients prefer attempting tooth preservation through apicoectomy before resorting to extraction and implantation.
The decision depends on individual circumstances, prognosis of the affected tooth, and long-term treatment goals. Dentists evaluate whether preserving the natural tooth through apicoectomy offers better long-term value than extraction followed by implant placement, considering factors like patient age, adjacent teeth condition, and bone quality.
Can Patients With Chronic Health Conditions Undergo Surgery?
Patients with chronic health conditions can often undergo apicoectomy, though careful evaluation and management are essential. Controlled diabetes patients are generally acceptable candidates, but uncontrolled diabetes significantly impairs healing and increases infection risk, requiring optimization before surgery.
Cardiovascular disease patients, including those on blood thinners, need medical consultation to balance bleeding risk against thromboembolic complications medication adjustments may be necessary. Immunocompromised patients from HIV, organ transplants, or chemotherapy face higher infection rates but can proceed with appropriate prophylactic measures.
Patients with bleeding disorders require hematological assessment and possible clotting factor replacement. Those with severe osteoporosis or taking bisphosphonates risk osteonecrosis, requiring careful risk-benefit analysis. Most chronic conditions don’t absolutely contraindicate apicoectomy but necessitate medical clearance, medication adjustments, antibiotic prophylaxis, or enhanced monitoring. Open communication between the dentist and patient’s physicians ensures safe treatment.
What Alternatives Exist if Apicoectomy Surgery Fails?
When apicoectomy fails, alternatives depend on the specific circumstances and tooth condition. The primary options include intentional replantation procedure where the tooth is carefully extracted, the root tip treated externally, then reimplanted though this carries significant risks and unpredictable outcomes.
Root amputation or hemi section might be considered for molars, removing only the problematic root while preserving the rest of the tooth. However, the most common outcome after apicoectomy failure is tooth extraction, as no further conservative treatments remain viable. Following extraction, patients face prosthetic replacement options including dental implants, fixed bridges, or removable partial dentures.
Some patients, particularly with posterior teeth that don’t affect appearance, choose to leave the space unfilled temporarily, though this isn’t recommended long-term due to tooth migration and bone loss. The treatment team discusses all options, considering patient preferences, budget, and overall oral health goals.
Can Retreatment of Root Canal Be Considered Before Apicoectomy?
Root canal retreatment should absolutely be considered before apicoectomy whenever feasible, as it’s less invasive and often successful. Retreatment involves removing the existing root canal filling material, re-cleaning and disinfecting the canal system, addressing any missed canals or inadequately cleaned areas, and refilling the canals.
This approach is preferred when the tooth crown is accessible without posts or extensive restorations blocking canal access. Studies show retreatment success rates of 70-85%, comparable to or sometimes better than apicoectomy. The procedure is typically less expensive and avoids surgical intervention.
However, retreatment isn’t always possible, posts extending deep into canals, severely calcified canals, separated instruments, or complex restorations like cores and crowns make canal access impractical or risk structural damage. When retreatment isn’t feasible or has already failed, apicoectomy becomes the next conservative option before considering extraction.
When Is Tooth Extraction the Only Option?
Tooth extraction becomes the only option when all conservative treatments have failed or are contraindicated. Specific scenarios necessitating extraction include vertical root fractures extending through the root, which cannot heal and cause persistent infection. Severe periodontal disease with extensive bone loss compromising tooth stability renders preservation futile.
When the tooth structure is insufficient to support a restoration long-term, maintaining it serves no purpose. Perforations in unfavorable locations that cannot be repaired may require extraction. If apicoectomy has failed and infection persists or recurs, extraction eliminates the chronic infection source. Financial constraints sometimes make extraction the only practical option when patients cannot afford complex procedures.
Teeth with poor long-term prognosis due to multiple factors even if technically savable may be better extracted. Patient preference also matters; some choose extraction over repeated procedures or ongoing problems, opting for definitive resolution through removal and replacement.
What Prosthetic Solutions Replace a Tooth After Extraction?
After tooth extraction, three primary prosthetic solutions restore function and appearance. Dental implants involve surgically placing a titanium post into the jawbone that integrates over 3-6 months, then attaching a custom crown that most closely mimics natural tooth function and prevents bone loss.
Fixed dental bridges use adjacent teeth as anchors, with a prosthetic tooth suspended between crowns placed on neighboring teeth, this avoids surgery but requires modifying healthy adjacent teeth. Removable partial dentures consist of prosthetic teeth attached to a gum-colored base with metal clasps securing to remaining teeth, these are least expensive and non-invasive but less stable and comfortable.
Each option has distinct advantages: implants preserve bone and don’t affect other teeth; bridges provide fixed, natural-feeling replacements without surgery; dentures offer economical, reversible solutions. The choice depends on patient health, bone quality, adjacent teeth condition, budget, and personal preferences regarding surgery and treatment complexity.
How Do Dental Implants Compare to Bridges After Extraction?
Dental implants and bridges each offer distinct advantages for replacing extracted teeth. Implants preserve the jawbone through osseointegration, preventing the bone resorption that occurs with tooth loss, while bridges don’t stimulate bone and can’t prevent underlying bone loss.
Implants stand independently without affecting adjacent teeth, whereas bridges require grinding down healthy neighboring teeth to serve as abutments, potentially compromising them. Longevity favors implants properly maintained implants can last 20+ years or lifetime, while bridges typically last 10-15 years before requiring replacement.
Cleaning is easier with implants as they function like natural teeth, while bridges require special flossing techniques under the pontin. However, bridges avoid surgical procedures, complete treatment faster (2-3 weeks versus 4-6 months), and cost less initially ($2,000-5,000 versus $3,000-6,000 per tooth). Bridge placement doesn’t depend on bone quality, while implants require adequate bone or preliminary grafting. The optimal choice depends on individual circumstances, priorities, and clinical factors.
Why Do International Patients Choose Turkey for Apicoectomy Surgery?
International patients choose Turkey for apicoectomy surgery due to a compelling combination of factors. Cost savings of 60-85% compared to Western countries represent the primary motivator, with quality remaining comparable or superior. Turkish dentists frequently train internationally, hold advanced degrees, and maintain memberships in prestigious organizations.
Modern clinics feature state-of-the-art equipment including surgical microscopes, 3D imaging, and latest materials. Many dental professionals speak excellent English, eliminating language barriers. Turkey’s strategic location bridging Europe and Asia offers convenient accessibility from multiple continents. The country’s developed medical tourism infrastructure provides comprehensive patient support including airport transfers, accommodation assistance, and translation services.
Patients appreciate combining dental treatment with tourism, exploring Turkey’s rich history, beautiful coastlines, and vibrant culture. Shorter waiting times compared to public healthcare systems in many European countries allow immediate treatment. Positive reviews and word-of-mouth recommendations from previous patients build confidence in Turkish dental care quality.
How Do Turkish Dental Clinics Ensure High Success Rates?
Turkish dental clinics ensure high apicoectomy success rates through multiple quality assurance mechanisms. Investment in advanced technology includes surgical operating microscopes providing up to 25x magnification, enabling precise identification of anatomy and thorough cleaning. CBCT 3D imaging allows detailed pre-operative planning, identifying anatomical variations and potential complications before surgery.
Clinics use premium materials like MTA and bio ceramics proven to have superior sealing properties and biocompatibility. Many Turkish endodontists pursue continuous education, attending international conferences, workshops, and certification programs to maintain cutting-edge knowledge. Strict sterilization protocols following international standards prevent infections. Clinics often follow evidence-based treatment protocols aligned with American or European endodontic association guidelines. Some facilities participate in international accreditation programs ensuring quality standards.
Comprehensive follow-up protocols with scheduled radiographic evaluations monitor healing. Many clinics track success rate data and patient satisfaction metrics, using outcomes to refine techniques. Experienced support staff and modern surgical suites contribute to optimal treatment conditions.
Why Is Turkey Known for Affordable and Quality Dental Care?
Turkey’s reputation for affordable, quality dental care stems from strategic national development in the healthcare and medical tourism sectors. The government has invested significantly in healthcare infrastructure and education, producing thousands of well-trained dental professionals annually from accredited universities. Turkey has 80+ dental schools, creating competitive markets that maintain reasonable pricing while driving quality improvements.
Many Turkish dentists pursue specialization or additional training abroad in countries like Germany, the US, or UK, then return bringing international standards and techniques. The country’s position as a medical tourism hub has fostered quality consciousness clinics understand international patients have choices and must deliver excellent results to maintain reputations.
Turkish dental associations enforce professional standards and continuing education requirements. The favorable cost structure allows investment in modern equipment while keeping prices accessible. International patients’ reviews and social media presence hold clinics accountable, incentivizing consistent quality. Cultural hospitality traditions extend to patient care, with attentive service and patient satisfaction prioritized.
What Role Does Dental Tourism Play in Apicoectomy Popularity?
Dental tourism significantly contributes to apicoectomy popularity in Turkey by making the procedure accessible to international patients who might otherwise delay or avoid treatment. The substantial cost savings justify travel expenses patients save thousands of dollars even after accounting for flights and accommodation.
Many patients strategically schedule dental appointments as part of vacation plans, transforming necessary medical procedures into positive experiences combining treatment with leisure. Medical tourism facilitators and agencies simplify the process, arranging comprehensive packages including consultations, treatment, accommodation, and sightseeing. Online reviews, forums, and social media groups share positive experiences, building trust and encouraging others to seek treatment abroad.
Turkey’s tourism infrastructure international airports, hotels, translation services makes the journey comfortable for foreigners. The country’s appeal as a travel destination with historical sites, beaches, and cultural attractions adds value beyond just dental savings. Dental tourism’s growth has pushed Turkish clinics to maintain high standards, invest in English-speaking staff, and develop patient-friendly protocols specifically catering to international visitors.
How Does Apicoectomy Surgery Support Other Dental Treatments?
Apicoectomy surgery supports other dental treatments by preserving tooth structure that serves as foundation for various restorative and cosmetic procedures. By saving teeth that would otherwise require extraction, apicoectomy maintains natural abutments for bridges, preserves dental arch integrity preventing orthodontic relapse, and keeps existing crowns, veneers, or other restorations functional.
The procedure eliminates chronic infections that could compromise adjacent teeth or implants, creating healthier oral environments for subsequent treatments. Apicoectomy allows completion of comprehensive treatment plans where tooth preservation is crucial for overall design, for instance, maintaining strategic teeth in full-mouth rehabilitation cases. The procedure prevents bone loss that would necessitate grafting before implant placement if extraction occurred.
Successfully treated teeth continue contributing to proper occlusion, distributing chewing forces appropriately and preventing excessive wear on remaining teeth. Apicoectomy essentially provides a stable foundation supporting complex, multi-faceted dental treatment plans by ensuring problematic teeth become assets rather than liabilities.
Can Apicoectomy Improve the Longevity of Dental Crowns?
Apicoectomy significantly improves dental crown longevity by eliminating underlying infections that would otherwise compromise the crowned tooth. Many crowns are placed on previously root canal-treated teeth; when these develop apical infections, the crown itself remains intact but the underlying tooth becomes compromised. Without apicoectomy, the infection would necessitate crown removal for retreatment or progress to tooth loss, wasting the crown investment.
By surgically resolving apical pathology without disturbing the crown, apicoectomy preserves both the tooth and its restoration. This is particularly valuable for expensive crowns made from all-ceramic or gold materials, or those that are part of bridge systems where replacement would require extensive additional work. The procedure allows crowned teeth to continue functioning indefinitely rather than failing prematurely.
Additionally, eliminating chronic inflammation prevents bone loss around the tooth, maintaining proper gum architecture and crown margin integrity. Apicoectomy essentially rescues the investment in crown treatment while extending the functional life of both restoration and tooth.
How Does Apicoectomy Complement Periodontal Therapy?
Apicoectomy complements periodontal therapy by addressing endodontic infections that can complicate or mimic periodontal disease. Some teeth develop combined endodontic-periodontal lesions where root canal infection drains through periodontal tissues, creating deep pockets resembling gum disease. Treating only the periodontal aspect without resolving the endodontic component results in treatment failure.
Apicoectomy eliminates the endodontic infection source, allowing periodontal tissues to heal properly after periodontal therapy. In cases where periodontal surgery is planned, coordinating apicoectomy timing ensures comprehensive infection control. The procedures can sometimes be performed simultaneously or staged appropriately. Resolving endodontic pathology creates healthier conditions for successful periodontal treatment outcomes.
Both treatments share goals of eliminating infection, preserving teeth, and maintaining healthy supporting structures. Patients undergoing comprehensive periodontal treatment programs benefit from addressing all infection sources, including apical lesions. The interdisciplinary approach considering both periodontal and endodontic health optimizes long-term tooth retention and overall oral health outcomes.
Can Apicoectomy Be Combined With Cosmetic Dentistry Procedures?
Apicoectomy can be strategically combined with cosmetic dentistry procedures, though timing and sequencing require careful planning. The procedure is often performed before cosmetic work when front teeth with aesthetic restorations develop apical infections resolving the infection first ensures the cosmetic investment isn’t compromised by underlying pathology.
Apicoectomy may be performed after cosmetic procedures if infections develop later, with the advantage of not disturbing expensive veneers or crowns during treatment. Some patients undergo apicoectomy as part of comprehensive smile makeover plans, ensuring all teeth are healthy before placing multiple veneers or crowns. The procedure’s focus on posterior surgical access typically doesn’t affect facial aesthetics or front tooth appearance.
However, in anterior teeth cases, surgeons carefully plan incisions to minimize visible scarring, sometimes coordinating with gum recontouring procedures. Patients pursuing full-mouth rehabilitation may need several apicoectomies to save strategic teeth essential to their treatment plan. The key is comprehensive diagnosis and treatment sequencing, ensuring both functional endodontic health and aesthetic goals are achieved harmoniously for optimal long-term results.
[sc_fs_multi_faq headline-0=”h3″ question-0=”What is the difference between apicoectomy and root canal treatment?” answer-0=”A root canal treats the inside of the tooth, while an apicoectomy removes the tip of the root and surrounding infected tissue when a root canal alone isn’t enough.” image-0=”” headline-1=”h3″ question-1=”How painful is apicoectomy surgery?” answer-1=”Most patients feel minimal pain during the procedure due to local anesthesia. Mild soreness or swelling afterward is common and manageable with medication.” image-1=”” headline-2=”h3″ question-2=”How long does it take to recover from apicoectomy?” answer-2=”Initial recovery takes 1–2 weeks. Full healing of the bone may take a few months.” image-2=”” headline-3=”h2″ question-3=”What is the success rate of apicoectomy in Turkey?” answer-3=”Success rates are high, generally between 85–95%, similar to international standards, especially when performed by experienced specialists.” image-3=”” headline-4=”h3″ question-4=”Can apicoectomy save a tooth with severe infection?” answer-4=”Yes, it can often save a tooth that hasn’t healed after a root canal or has a persistent infection.” image-4=”” headline-5=”h3″ question-5=”Is apicoectomy surgery safe for older patients?” answer-5=”Yes, it’s generally safe for older adults, provided there are no serious underlying health conditions.” image-5=”” headline-6=”h3″ question-6=”How much does apicoectomy cost in Turkey compared to Europe?” answer-6=”Apicoectomy in Turkey is significantly more affordable, often costing 50–70% less than in Western Europe.” image-6=”” headline-7=”h3″ question-7=”Can apicoectomy be performed on molars?” answer-7=”Yes, but it’s more complex due to molar anatomy. Still, skilled endodontists can perform it successfully.” image-7=”” headline-8=”h3″ question-8=”What should I eat after apicoectomy surgery?” answer-8=”Eat soft, non-spicy, and non-acidic foods like yogurt, mashed potatoes, soups, and smoothies. Avoid chewing on the surgery side.” image-8=”” headline-9=”h3″ question-9=”Are there long-term risks after apicoectomy?” answer-9=”Long-term risks are rare. In some cases, the infection may return, or the tooth may still require extraction later.” image-9=”” count=”10″ html=”true” css_class=””]