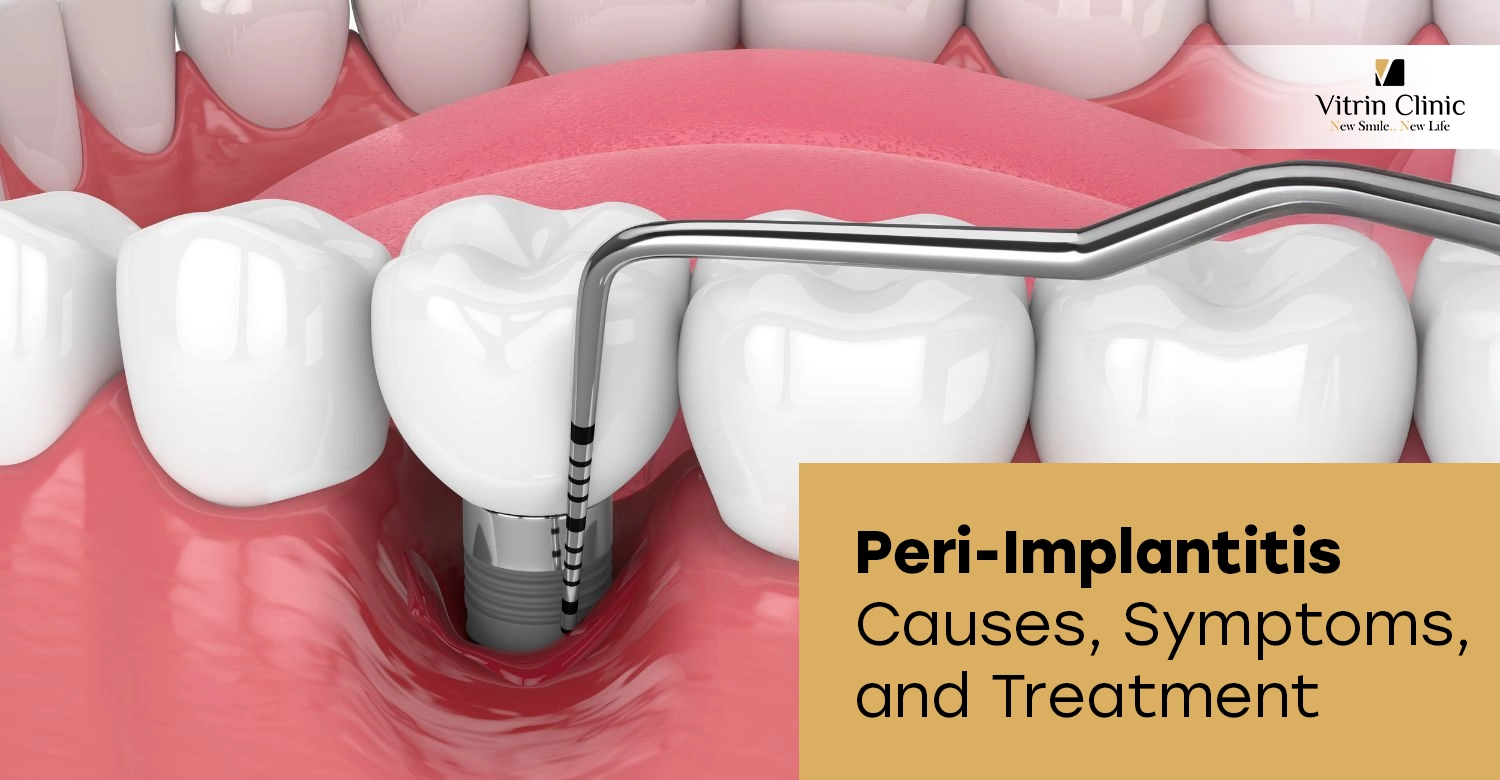
Peri-implantitis is a destructive inflammatory condition affecting tissues surrounding dental implants, causing bone loss and potential implant failure. This peri-implantitis dental implant infection results from bacterial accumulation, poor oral hygiene, and various risk factors. Understanding peri-implantitis symptoms, peri-implantitis causes, and available peri-implantitis treatment options helps patients protect their dental implant investments and maintain long-term oral health through proper prevention strategies and timely intervention.
Understanding Peri-Implantitis
Peri-implantitis is a progressive inflammatory disease affecting bone and soft tissues surrounding dental implants. This peri-implantitis dental implant infection involves bacterial colonization causing tissue destruction and bone resorption. Understanding what causes peri-implantitis and recognizing peri-implantitis symptoms early enables effective intervention. Without proper peri-implantitis treatment, the condition progresses through stages of peri-implantitis, ultimately threatening implant stability and survival. Comprehensive knowledge about peri-implantitis prevention helps patients maintain healthy implants long-term.
What Is Peri-Implantitis?
Peri-implantitis is a pathological condition characterized by inflammation of soft tissues around dental implants accompanied by progressive bone loss. This peri-implantitis dental implant infection occurs when bacteria accumulate on implant surfaces, triggering immune responses that destroy supporting bone. Unlike reversible peri-implant mucositis, peri-implantitis involves irreversible bone damage requiring immediate peri-implantitis treatment. The condition affects 10-20% of implants, making understanding peri-implantitis causes and peri-implantitis prevention crucial for implant success.
How Peri-Implantitis Affects Dental Implants
Peri-implantitis affects dental implants by destroying surrounding bone that provides support and stability for implant fixtures. The peri-implantitis dental implant infection creates pockets between implant and tissue, harboring bacteria and inflammation. Progressive bone loss through stages of peri-implantitis weakens implant anchorage, causing mobility and eventual failure. Untreated peri-implantitis symptoms worsen over time, requiring increasingly invasive peri-implantitis treatment approaches. Understanding how peri-implantitis develops emphasizes the importance of peri-implantitis prevention and regular maintenance.
Peri-Implantitis vs Peri-Implant Mucositis
Peri-implantitis vs peri-implant mucositis represents a crucial distinction in implant complications, differing in bone involvement and reversibility. Peri-implant mucositis affects only soft tissues without bone loss, remaining reversible with proper treatment. Peri-implantitis involves progressive bone destruction, requiring more aggressive peri-implantitis treatment interventions. Recognizing differences between conditions enables appropriate responses to peri-implantitis symptoms. Early detection prevents progression from mucositis to peri-implantitis, emphasizing importance of peri-implantitis prevention and regular professional monitoring.
Key Differences Between Peri-Implantitis and Mucositis
Key differences in peri-implantitis vs peri-implant mucositis include bone loss presence and disease reversibility. Mucositis shows inflammation, bleeding, and swelling without bone destruction, responding well to improved hygiene. Peri-implantitis demonstrates these peri-implantitis symptoms plus progressive bone loss visible on radiographs, requiring professional peri-implantitis treatment. Mucositis remains reversible; peri-implantitis causes permanent bone damage. Understanding stages of peri-implantitis helps differentiate conditions, guiding appropriate intervention and emphasizing peri-implantitis prevention importance.
Why Early Detection Matters
Early detection of peri-implantitis matters because initial stages of peri-implantitis respond better to non-surgical treatment for peri-implantitis with higher success rates. Recognizing early peri-implantitis symptoms enables intervention before extensive bone loss occurs, improving prognosis significantly. Delayed peri-implantitis treatment allows progression through advanced stages of peri-implantitis, requiring surgical intervention or implant removal. Regular monitoring identifies peri-implantitis dental implant infection early, reducing peri-implantitis treatment cost and preserving implants. Proper peri-implantitis prevention includes scheduled professional evaluations detecting problems promptly.
Peri-Implantitis Causes
Peri-implantitis causes include bacterial biofilm accumulation, poor oral hygiene, smoking, diabetes, and history of periodontal disease. Understanding what triggers peri-implantitis dental implant infection helps patients avoid risk factors through effective peri-implantitis prevention strategies. Multiple factors often combine, accelerating progression through stages of peri-implantitis. Identifying individual peri-implantitis causes enables personalized prevention approaches and appropriate peri-implantitis treatment planning. Addressing underlying causes improves treatment outcomes and reduces recurrence risk significantly.
Common Risk Factors for Peri-Implantitis
Common risk factors for peri-implantitis include smoking, which reduces blood flow and immune response, increasing infection susceptibility. Diabetes impairs healing and infection resistance, elevating peri-implantitis dental implant infection risk. Previous periodontal disease indicates bacterial susceptibility, making patients prone to peri-implantitis causes. Poor oral hygiene allows biofilm accumulation triggering inflammation. Excess cement residue from restorations harbors bacteria contributing to peri-implantitis symptoms. Genetic factors and inadequate keratinized tissue also influence peri-implantitis development, affecting peri-implantitis prevention effectiveness.
How Poor Oral Hygiene and Systemic Conditions Contribute
Poor oral hygiene contributes to peri-implantitis by allowing bacterial plaque accumulation on implant surfaces, initiating peri-implantitis dental implant infection. Inadequate cleaning creates biofilms triggering inflammatory responses that progress through stages of peri-implantitis. Systemic conditions like diabetes compromise immune function, reducing ability to control bacteria causing peri-implantitis symptoms. Cardiovascular disease and osteoporosis affect bone metabolism, influencing how to treat peri-implantitis effectively. Combined local and systemic peri-implantitis causes require comprehensive approaches addressing both oral hygiene and medical management.
Peri-Implantitis Symptoms
Peri-implantitis symptoms include bleeding on probing, gum inflammation, suppuration, increased pocket depths, and progressive bone loss around implants. Recognizing early peri-implantitis symptoms enables timely intervention before advanced stages of peri-implantitis develop. Patients may notice swelling, redness, pain, or implant mobility indicating peri-implantitis dental implant infection. Understanding these warning signs facilitates prompt peri-implantitis treatment, improving success rates. Regular monitoring detects subtle peri-implantitis symptoms before severe complications occur, emphasizing importance of professional maintenance and peri-implantitis prevention strategies.
Early Warning Signs of Peri-Implant Disease
Early warning signs of peri-implantitis include bleeding when brushing or flossing around implants, indicating initial inflammation. Gum redness and swelling around implant crowns suggest developing peri-implantitis symptoms requiring evaluation. Mild discomfort or sensitivity indicates possible peri-implantitis dental implant infection beginning. Increased pocket depths detected during professional examinations reveal early stages of peri-implantitis. These subtle signs warrant immediate attention for non-surgical treatment for peri-implantitis, preventing progression to advanced disease requiring surgical intervention and reducing overall peri-implantitis treatment cost.
Advanced Symptoms and Implant Complications
Advanced peri-implantitis symptoms include visible pus discharge, severe gum recession exposing implant threads, and significant implant mobility. Patients experience persistent pain, difficulty chewing, and foul taste indicating severe peri-implantitis dental implant infection. Radiographs reveal extensive bone loss characterizing advanced stages of peri-implantitis. Tissue inflammation becomes pronounced with deep periodontal pockets around implants. These complications necessitate aggressive peri-implantitis treatment approaches including surgical intervention. Without treatment, advanced peri-implantitis causes implant failure requiring removal, emphasizing critical importance of peri-implantitis prevention.
Stages of Peri-Implantitis
Stages of peri-implantitis progress from early inflammation with minimal bone loss to moderate disease with increasing bone destruction, culminating in advanced stages threatening implant survival. Understanding progression helps determine appropriate peri-implantitis treatment approaches and prognosis. Early stages of peri-implantitis respond well to non-surgical treatment for peri-implantitis, while advanced cases require surgical intervention. Recognizing which stage the patient presents guides how to treat peri-implantitis effectively. Regular monitoring prevents progression through stages of peri-implantitis, emphasizing peri-implantitis prevention importance in maintaining implant health.
Early, Moderate, and Advanced Stages Explained
Early stages of peri-implantitis show initial bone loss (1-3mm) with bleeding, swelling, and pocket formation, responding well to non-surgical treatment for peri-implantitis. Moderate peri-implantitis demonstrates 3-5mm bone loss with increased inflammation and peri-implantitis symptoms including suppuration. Advanced stages of peri-implantitis involve severe bone destruction exceeding 5mm, implant mobility, and extensive tissue damage requiring surgical peri-implantitis treatment. Each stage represents progression of peri-implantitis dental implant infection severity, directly affecting prognosis and determining appropriate intervention approaches.
How Disease Progression Affects Implant Stability
Disease progression through stages of peri-implantitis directly compromises implant stability by destroying supporting bone tissue surrounding fixtures. Early peri-implantitis causes minimal stability loss, remaining manageable with conservative peri-implantitis treatment. Moderate progression reduces bone-to-implant contact significantly, affecting load distribution and causing discomfort. Advanced peri-implantitis symptoms include noticeable mobility, pain during function, and potential implant failure. Progressive bone loss from peri-implantitis dental implant infection eliminates anchorage, making implant removal necessary. Understanding how progression affects stability emphasizes critical importance of early intervention and peri-implantitis prevention.
How to Treat Peri-Implantitis
How to treat peri-implantitis depends on disease severity, ranging from non-surgical treatment for peri-implantitis in early cases to surgical intervention for advanced stages. Effective peri-implantitis treatment requires comprehensive diagnosis, risk factor control, and appropriate therapeutic approaches based on stages of peri-implantitis. Treatment goals include eliminating peri-implantitis dental implant infection, resolving inflammation, and arresting bone loss. Understanding available options helps patients make informed decisions about peri-implantitis treatment approaches. Success rates vary with disease severity, emphasizing importance of addressing peri-implantitis symptoms early.
Diagnosis and Treatment Planning
Diagnosis of peri-implantitis involves clinical examination assessing peri-implantitis symptoms including bleeding, suppuration, and increased probing depths around implants. Radiographic evaluation reveals bone loss extent, determining stages of peri-implantitis. Comprehensive assessment identifies peri-implantitis causes including risk factors requiring management. Treatment planning for how to treat peri-implantitis considers disease severity, patient health, and implant characteristics. Proper diagnosis guides selection between non-surgical treatment for peri-implantitis versus surgical approaches, affecting overall peri-implantitis treatment cost and expected outcomes significantly.
When Immediate Treatment Is Necessary
Immediate peri-implantitis treatment becomes necessary when patients present with acute symptoms including severe pain, extensive swelling, or purulent discharge from peri-implantitis dental implant infection. Rapid bone loss progression through stages of peri-implantitis requires urgent intervention preventing implant failure. Systemic symptoms like fever indicate serious infection demanding immediate attention. Implant mobility signals advanced disease necessitating prompt evaluation of how to treat peri-implantitis. Delaying treatment allows progression of peri-implantitis and causes additional bone destruction, reducing success rates and potentially requiring implant removal.
Non-Surgical Treatment for Peri-Implantitis
Non-surgical treatment for peri-implantitis effectively manages early stages of peri-implantitis through mechanical debridement, antimicrobial therapy, and improved oral hygiene protocols. This conservative approach to how to treat peri-implantitis removes bacterial biofilms causing peri-implantitis dental implant infection without surgical intervention. Treatment includes professional cleaning, laser therapy, and chemical decontamination of implant surfaces. Non-surgical peri-implantitis treatment proves most effective when addressing initial peri-implantitis symptoms before extensive bone loss occurs, offering lower peri-implantitis treatment cost and faster recovery compared to surgical approaches.
Deep Cleaning and Implant Surface Decontamination
Deep cleaning for peri-implantitis treatment involves mechanical debridement removing bacterial biofilms and calculus from implant surfaces causing peri-implantitis dental implant infection. Specialized instruments including plastic curettes, ultrasonic scalers, and air-abrasive devices decontaminate without damaging implant threads. Laser therapy provides additional antimicrobial benefits in non-surgical treatment for peri-implantitis. Chemical agents like chlorhexidine or hydrogen peroxide further disinfect surfaces. This approach effectively addresses early peri-implantitis symptoms, controlling inflammation and arresting progression through stages of peri-implantitis when combined with improved hygiene.
Medications and Antimicrobial Therapies
Medications for peri-implantitis treatment include systemic antibiotics targeting bacteria causing peri-implantitis dental implant infection when systemic involvement exists. Local antimicrobial agents applied directly into pockets provide concentrated therapy for non-surgical treatment for peri-implantitis. Chlorhexidine rinses control bacterial populations reducing peri-implantitis symptoms. Anti-inflammatory medications manage tissue response. Probiotic therapy shows promise in supporting peri-implantitis prevention. While medications support how to treat peri-implantitis, they supplement rather than replace mechanical debridement, working synergistically for optimal outcomes in managing peri-implantitis causes.
Surgical Peri-Implantitis Treatment
Surgical peri-implantitis treatment addresses moderate to advanced stages of peri-implantitis when non-surgical treatment for peri-implantitis proves insufficient. Surgical approaches to how to treat peri-implantitis include access flap surgery for thorough decontamination, resective procedures removing damaged tissue, and regenerative techniques attempting bone regrowth. Advanced peri-implantitis symptoms requiring surgical intervention indicate significant bone loss and deep pocket formation. Surgical peri-implantitis treatment provides direct visualization and access for complete biofilm removal from peri-implantitis dental implant infection, improving outcomes in severe cases despite higher peri-implantitis treatment cost.
A successful outcome involves understanding and mitigating potential dental implant complications
Surgical Cleaning and Bone Regeneration
Surgical cleaning for peri-implantitis treatment involves flap elevation providing direct access to contaminated implant surfaces for thorough decontamination. Granulation tissue removal eliminates infection reservoirs in peri-implantitis dental implant infection. Implant surface treatment using mechanical, chemical, or laser methods removes biofilms. Bone regeneration attempts using grafts and membranes aim to restore lost bone in stages of peri-implantitis. While regenerative outcomes remain unpredictable for how to treat peri-implantitis, resective surgery creating maintainable contours shows more reliable results in managing advanced peri-implantitis symptoms.
When Implant Removal Becomes Necessary
Implant removal becomes necessary when severe peri-implantitis causes extensive bone loss preventing successful treatment or implant mobility compromising function. Advanced stages of peri-implantitis with progressive destruction despite aggressive peri-implantitis treatment warrant explanation. Persistent peri-implantitis symptoms including pain, suppuration, and infection unresponsive to surgical intervention indicate removal necessity. Implant fracture, severe positioning problems, or patient health concerns may necessitate extraction. While removal represents peri-implantitis treatment failure, it prevents continued bone loss, allowing future implant placement after adequate healing and addressing underlying peri-implantitis causes.
Peri-Implantitis Treatment Cost
Peri-implantitis treatment cost varies significantly based on disease severity, chosen treatment approach, and geographic location. Non-surgical treatment for peri-implantitis typically costs $500-$1,500 per implant for mechanical debridement and antimicrobial therapy. Surgical peri-implantitis treatment ranges $1,500-$5,000 depending on complexity and regenerative procedures used. Understanding factors affecting peri-implantitis treatment cost helps patients budget appropriately. International options like Vitrin Clinic in Turkey offer comprehensive peri-implantitis treatment at 60-70% reduced costs while maintaining quality standards, making advanced care accessible for managing peri-implantitis dental implant infection.
Average Cost of Treating Peri-Implantitis
Average peri-implantitis treatment cost ranges $500-$1,500 for non-surgical treatment for peri-implantitis including professional debridement and antimicrobial therapy per implant. Surgical intervention for how to treat peri-implantitis costs $1,500-$3,000 for access surgery and decontamination. Regenerative procedures attempting bone restoration increase peri-implantitis treatment cost to $2,500-$5,000 per implant. Multiple implants with peri-implantitis symptoms require proportionally higher investment. Implant removal and replacement exceed $5,000 total. Turkey offers comprehensive peri-implantitis treatment addressing peri-implantitis dental implant infection at significantly reduced prices while maintaining international standards.
Factors That Influence Treatment Pricing
Factors influencing peri-implantitis treatment cost include disease severity with advanced stages of peri-implantitis requiring more complex, expensive interventions than early disease. Surgical versus non-surgical treatment for peri-implantitis significantly affects pricing. Geographic location impacts fees substantially. Specialist experience and clinic technology influence costs. The number of affected implants multiplies expenses. Regenerative materials for bone grafting increase peri-implantitis treatment cost. Follow-up care and maintenance programs add ongoing expenses. Insurance coverage varies widely. Addressing underlying peri-implantitis causes like smoking cessation or diabetes management may require additional investments affecting total treatment costs.
Peri-Implantitis Prevention
Peri-implantitis prevention involves meticulous daily oral hygiene, regular professional maintenance, and risk factor management to prevent peri-implantitis dental implant infection development. Effective prevention strategies reduce incidence of peri-implantitis symptoms and progression through stages of peri-implantitis. Proper cleaning techniques, specialized tools, and consistent professional monitoring maintain implant health long-term. Understanding peri-implantitis causes targeted prevention approaches. Investment in peri-implantitis prevention proves more cost-effective than managing established disease requiring extensive peri-implantitis treatment. Comprehensive prevention programs support implant longevity and patient satisfaction.
A resin-bonded or adhesive bridge offers a less invasive alternative to traditional bridges
Daily Oral Care Tips for Implant Health
Daily oral care for peri-implantitis prevention includes brushing implant crowns and surrounding tissues twice daily using soft-bristled toothbrushes or electric brushes. Interdental cleaning with floss, interdental brushes, or water flossers removes plaque preventing peri-implantitis dental implant infection. Antimicrobial mouth rinses provide additional protection against bacteria causing peri-implantitis symptoms. Non-abrasive toothpaste prevents surface damage. Proper technique ensures thorough cleaning without traumatizing tissues. Consistent home care represents primary defense against peri-implantitis causes, significantly reducing risk of disease development and need for peri-implantitis treatment interventions.
Importance of Regular Dental Implant Maintenance
Regular dental implant maintenance proves critical for peri-implantitis prevention through professional monitoring detecting early peri-implantitis symptoms before extensive damage occurs. Scheduled cleanings remove calculus and biofilms patients cannot eliminate, preventing peri-implantitis dental implant infection. Professional evaluations assess tissue health, probing depths, and bone levels, identifying progression through stages of peri-implantitis. Maintenance visits enable risk factor assessment and modification addressing peri-implantitis causes. Frequency typically ranges 3-6 months depending on individual risk. Consistent professional care dramatically reduces disease incidence, avoiding extensive non-surgical treatment for peri-implantitis or surgical interventions.
Why Choose Vitrin Clinic for Peri-Implantitis Treatment
Vitrin Clinic in Istanbul, Turkey offers comprehensive peri-implantitis treatment combining advanced diagnostics, experienced specialists, and proven protocols for managing peri-implantitis dental implant infection. Our team excels in both non-surgical treatment for peri-implantitis and surgical interventions for advanced stages of peri-implantitis. We provide personalized approaches based on individual peri-implantitis causes and peri-implantitis symptoms. Vitrin Clinic delivers international-quality care at significantly reduced peri-implantitis treatment cost, making advanced implant infection management accessible. Our focus on peri-implantitis prevention and long-term maintenance ensures optimal implant health and patient satisfaction.
Advanced Diagnostics and Implant Infection Management at Vitrin Clinic
Vitrin Clinic utilizes advanced 3D CBCT imaging for precise evaluation of bone loss and stages of peri-implantitis, enabling accurate diagnosis of peri-implantitis dental implant infection. Comprehensive assessment identifies specific peri-implantitis causes requiring management. Our diagnostic protocols detect subtle peri-implantitis symptoms early, allowing conservative non-surgical treatment for peri-implantitis with higher success rates. State-of-the-art equipment supports both surgical and non-surgical approaches to how to treat peri-implantitis. Digital planning optimizes treatment outcomes while minimizing invasiveness. Advanced diagnostics at Vitrin Clinic ensure appropriate, effective interventions for managing peri-implantitis at reasonable peri-implantitis treatment cost.
Experienced Specialists Focused on Saving Dental Implants
Vitrin Clinic’s experienced specialists focus on implant preservation through evidence-based peri-implantitis treatment protocols addressing peri-implantitis dental implant infection effectively. Our periodontists and implantologists have extensive training in managing all stages of peri-implantitis using both non-surgical treatment for peri-implantitis and advanced surgical techniques. We emphasize conservative approaches when possible, reserving invasive procedures for severe cases. Our team addresses underlying peri-implantitis causes including patient education for peri-implantitis prevention. Comprehensive care at Vitrin Clinic maximizes implant salvage rates while providing affordable peri-implantitis treatment cost, helping patients preserve their dental implant investments successfully.
Budgeting for your new smile starts with understanding snap-in dentures cost
Conclusion
Peri-implantitis represents a serious threat to dental implant longevity, requiring understanding of peri-implantitis causes, recognition of peri-implantitis symptoms, and prompt intervention. Effective peri-implantitis treatment ranges from non-surgical treatment for peri-implantitis in early cases to surgical intervention for advanced stages of peri-implantitis. Prevention through proper oral hygiene and regular maintenance proves the most effective strategy. Vitrin Clinic offers comprehensive care for managing peri-implantitis dental implant infection at accessible peri-implantitis treatment cost, helping patients preserve their implants and oral health.
Key Takeaways About Peri-Implantitis
Peri-implantitis involves inflammatory disease causing progressive bone loss around dental implants from peri-implantitis dental implant infection. Understanding peri-implantitis causes including poor hygiene, smoking, and systemic conditions enables effective peri-implantitis prevention. Recognizing early peri-implantitis symptoms allows timely intervention with non-surgical treatment for peri-implantitis. Advanced stages of peri-implantitis require surgical intervention or potential implant removal. Regular professional maintenance and excellent home care represent primary defense. Peri-implantitis treatment cost varies but remains more affordable than implant replacement, especially at Vitrin Clinic in Turkey.
Early Treatment at Vitrin Clinic Can Help Save Your Dental Implant
Early peri-implantitis treatment at Vitrin Clinic maximizes chances of saving affected dental implants through prompt intervention addressing peri-implantitis dental implant infection. Our specialists identify peri-implantitis symptoms early, implementing appropriate non-surgical treatment for peri-implantitis before extensive bone loss occurs. We address underlying peri-implantitis causes and provide comprehensive peri-implantitis prevention education. Advanced diagnostics guide optimal approaches for how to treat peri-implantitis at each stage. Accessible peri-implantitis treatment cost at Vitrin Clinic makes quality care affordable. Contact us today to protect your dental implant investment through expert management and prevention strategies.
FAQs
What is peri-implantitis and how serious is it?
Peri-implantitis is an inflammatory disease causing progressive bone loss around dental implants from bacterial peri-implantitis dental implant infection. The condition proves serious because untreated disease progresses through stages of peri-implantitis, ultimately causing implant failure requiring removal. Unlike reversible mucositis, peri-implantitis causes permanent bone destruction. Approximately 10-20% of implants develop peri-implantitis symptoms requiring professional intervention. Severity depends on extent and progression rate. Early detection and appropriate peri-implantitis treatment significantly improve prognosis. Without treatment, peri-implantitis threatens implant survival and surrounding bone structure.
Experience superior stability and comfort with modern permanent dentures
What are the early symptoms of peri-implantitis?
Early peri-implantitis symptoms include bleeding when brushing or flossing around implants, indicating inflammation from developing peri-implantitis dental implant infection. Patients notice gum redness, swelling, and tenderness surrounding implant crowns. Mild discomfort or sensitivity suggests initial tissue involvement. Professional examination reveals increased pocket depths and bleeding on probing. These subtle signs in early stages of peri-implantitis require immediate attention for successful non-surgical treatment for peri-implantitis. Recognizing these warning signals enables intervention before extensive bone loss develops, improving treatment outcomes and reducing overall peri-implantitis treatment cost significantly.
How is peri-implantitis different from peri-implant mucositis?
Peri-implantitis vs peri-implant mucositis differs primarily in bone involvement and reversibility. Mucositis affects only soft tissues showing inflammation, bleeding, and swelling without bone loss, remaining fully reversible with improved hygiene. Peri-implantitis involves progressive bone destruction visible on radiographs, representing irreversible damage requiring professional peri-implantitis treatment. Mucositis serves as a precursor to peri-implantitis if untreated. Both show similar initial peri-implantitis symptoms including inflammation and bleeding, but peri-implantitis causes permanent structural damage progressing through stages of peri-implantitis. Early intervention prevents mucositis progression to peri-implantitis dental implant infection.
Can peri-implantitis be treated without surgery?
Non-surgical treatment for peri-implantitis effectively manages early stages of peri-implantitis through mechanical debridement removing bacterial biofilms causing peri-implantitis dental implant infection. Treatment includes professional cleaning, antimicrobial therapy, laser decontamination, and improved oral hygiene protocols. Success depends on disease severity, with early peri-implantitis symptoms responding better than advanced cases. Studies show 40-60% success rates for non-surgical approaches in early disease. However, moderate to advanced stages of peri-implantitis typically require surgical intervention for adequate decontamination. Conservative how to treat peri-implantitis approaches work best when addressing peri-implantitis causes early.
What causes peri-implantitis around dental implants?
Peri-implantitis causes include bacterial biofilm accumulation triggering inflammatory responses destroying bone around implants creating peri-implantitis dental implant infection. Poor oral hygiene allows plaque buildup initiating disease. Smoking reduces blood flow and immune response, significantly increasing risk. Diabetes impairs healing and infection resistance. History of periodontal disease indicates bacterial susceptibility. Excess cement residue from restorations harbors bacteria contributing to peri-implantitis symptoms. Inadequate keratinized tissue, genetic factors, and implant design influence development. Understanding these peri-implantitis causes enables targeted peri-implantitis prevention strategies reducing disease incidence effectively.
How much does peri-implantitis treatment cost?
Peri-implantitis treatment cost varies based on disease severity and intervention type. Non-surgical treatment for peri-implantitis typically costs $500-$1,500 per implant including debridement and antimicrobial therapy. Surgical intervention for how to treat peri-implantitis ranges $1,500-$3,000 for access surgery and decontamination. Regenerative procedures attempting bone restoration increase costs to $2,500-$5,000 per implant. Multiple affected implants multiply expenses proportionally. Geographic location significantly impacts pricing. Vitrin Clinic in Turkey offers comprehensive peri-implantitis treatment for peri-implantitis dental implant infection at 60-70% reduced costs while maintaining international quality standards and experienced specialists.
Can peri-implantitis be cured completely?
Complete cure of peri-implantitis remains challenging because bone loss from peri-implantitis dental implant infection is irreversible, though disease progression can be arrested. Successful peri-implantitis treatment aims to eliminate infection, resolve inflammation, and stabilize bone levels preventing further destruction. Non-surgical treatment for peri-implantitis controls early stages effectively. Surgical intervention manages advanced disease but cannot fully restore lost bone. Treatment success rates vary with disease severity and patient compliance. While complete restoration to pre-disease state rarely occurs, appropriate intervention addressing peri-implantitis causes and maintaining proper peri-implantitis prevention protocols enables long-term implant retention.
How can peri-implantitis be prevented?
Peri-implantitis prevention requires meticulous daily oral hygiene including thorough brushing and interdental cleaning removing plaque preventing peri-implantitis dental implant infection development. Use specialized tools like interdental brushes and water flossers for implant areas. Regular professional maintenance every 3-6 months enables early detection of peri-implantitis symptoms and removal of calculus patients cannot eliminate. Smoking cessation dramatically reduces risk among key peri-implantitis causes. Managing systemic conditions like diabetes improves infection resistance. Proper implant design, adequate keratinized tissue, and cement removal during restoration prevent disease. Consistent home care and professional monitoring represent most effective peri-implantitis prevention strategies.