The vast majority of bone graft procedures are completed without a hitch, but like any surgical procedure, there are common risks involved. These are often minor and temporary, yet they are important for patients to be aware of before committing to the surgery. The most common issues include localized swelling, bruising, and some degree of post-operative pain. Another frequent concern is a low-grade fever, which is a normal immune response to the surgical trauma but can be alarming if you’re not expecting it.
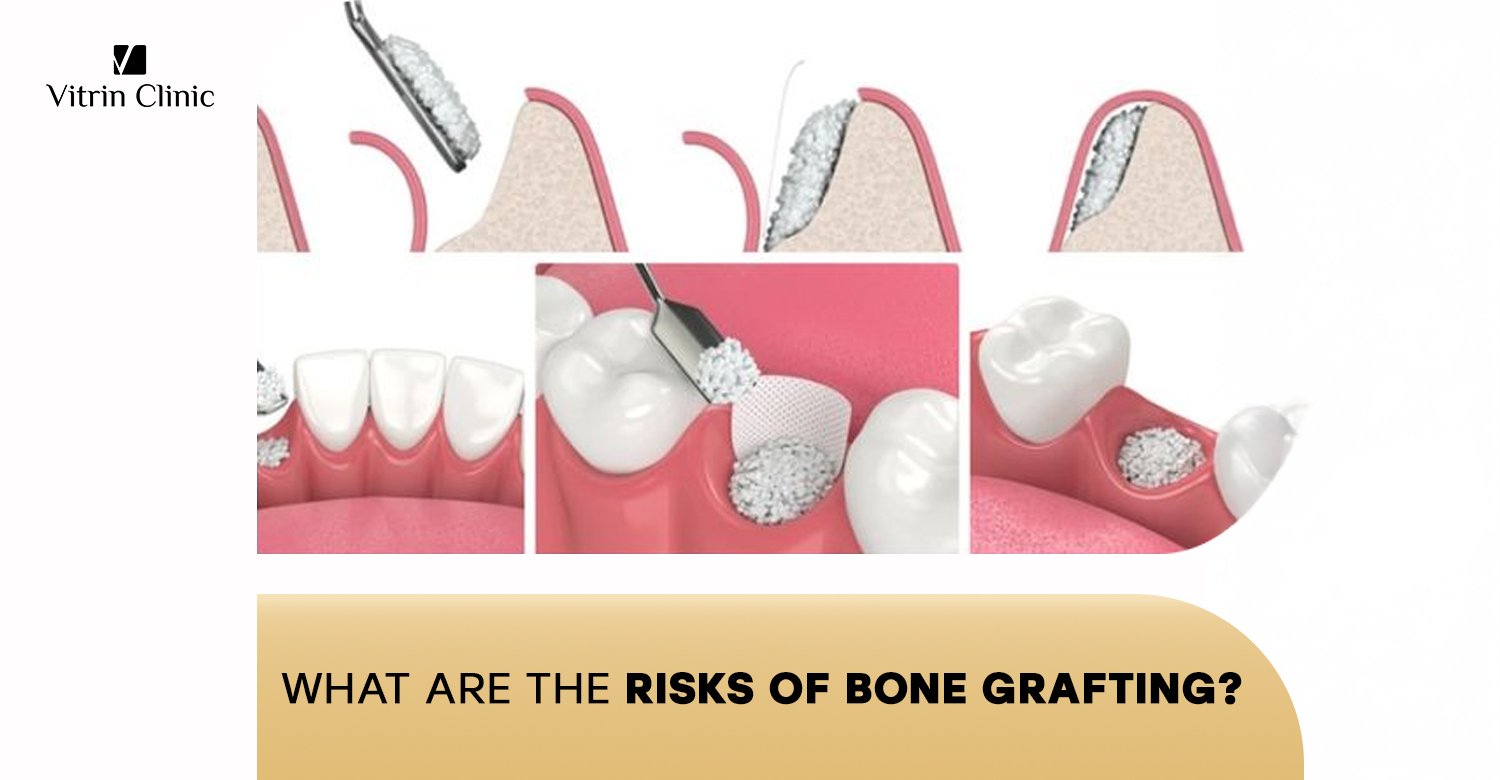
What Immediate Complications Can Occur During Bone Grafting Surgery?
During the procedure itself, a few immediate complications can arise, although they are rare. These are typically handled by the surgical team as they happen, minimizing any long-term effects. A significant concern for many is the possibility of excessive bleeding, which is why your surgeon will review your medical history, especially if you’re on blood thinners. Nerve damage is another potential, though very infrequent, risk that can result in temporary or, in extremely rare cases, permanent numbness.
How Common Is Excessive Bleeding During The Procedure?
Excessive bleeding during a bone graft procedure is not a common occurrence. Surgeons take meticulous care to ensure blood vessels are managed and to minimize blood loss throughout the operation. For patients who are taking blood-thinning medications, their doctor will typically advise them to stop a few days before the surgery to reduce this risk. The surgeon’s expertise and careful technique are key to preventing this issue, making significant bleeding a rare event.
What Causes Nerve Damage During Bone Graft Surgery?
Nerve damage during bone grafting is a rare complication that primarily occurs when the surgical site is in close proximity to a major nerve, such as the inferior alveolar nerve in the lower jaw. The cause is usually accidental trauma to the nerve during drilling or manipulation of the jawbone. While most nerve-related issues are temporary and resolve on their own
Can Anesthesia Complications Occur During Bone Grafting?
Anesthesia complications, while uncommon, are a risk with any surgical procedure. They can range from minor side effects like nausea or dizziness to more serious, life-threatening issues, although the latter is extremely rare with modern anesthesia protocols. Patients with pre-existing conditions like heart or lung issues are at a slightly higher risk, which is why a thorough medical evaluation is a mandatory part of the pre-operative process.
What Post-Operative Risks Should Patients Expect After Bone Grafting?
Once the surgery is complete, the focus shifts to managing post-operative risks, which are far more common than immediate surgical complications. These include pain, swelling, and bruising, all of which are a normal part of the body’s healing response. While most of these symptoms are temporary and manageable, it’s crucial to know what to look for that might signal a problem. A minor fever is also common in the first 24-48 hours. The most important thing is to follow your surgeon’s aftercare instructions precisely to minimize the risks of bone grafting and ensure a smooth recovery.
How Long Does Post-Surgical Pain Typically Last?
Post-surgical pain from a bone graft typically lasts for the first few days after the procedure. It is usually most intense during the first 24 to 48 hours and then gradually subsides. Your surgeon will prescribe pain medication to help you manage this discomfort, and many patients find that over-the-counter pain relievers are sufficient after the initial period.
What Signs Indicate Abnormal Swelling After Surgery?
Normal swelling after bone grafting usually peaks within 2 to 3 days and then begins to decrease. However, abnormal swelling might be a sign of a problem, particularly if it is severe, extends beyond the immediate surgical area, or is accompanied by increasing pain and redness. This could indicate an infection or a hematoma.
When Should Patients Be Concerned About Bruising?
Bruising around the surgical site is a very common and normal side effect of bone grafting. It is a result of bleeding under the skin and usually appears as a blue or purple discoloration that fades to yellow or green over time. You should be concerned about bruising if it is severe, spreads rapidly, or is accompanied by other signs of a complication, such as a high fever or pus. Normal bruising typically resolves within 1 to 2 weeks. The bone graft recovery process requires patience, but it is essential for successful implant placement
What Are The Signs Of Bone Graft Infection?
If you’ve had a dental bone graft, it’s important to watch for symptoms that may indicate infection or graft failure. Key warning signs include:
- Increasing pain after the first few days instead of gradual improvement.
- Severe or worsening swelling around the surgical area.
- Redness of the gums or surrounding tissue that continues or intensifies.
- Bad taste or foul odor coming from the surgical site.
- Pus or discharge from the graft area.
- Persistent or rising fever, especially beyond the first couple of days.
- Delayed healing or the wound not closing properly.
Tip: Contact your dentist or oral surgeon immediately if you notice any of these symptoms to prevent.
How Can Patients Identify Early Infection Symptoms?
During the first week of recovery, be alert for subtle warning signs, such as:
- Pain that worsens instead of improving, especially if it feels pulsating or throbbing.
- Persistent redness around the surgical area that does not fade.
- Swelling continues to increase after the third day rather than gradually decreasing.
- Foul odor or bad taste in the mouth, which may signal pus or bacterial growth.
- Increased warmth or tenderness around the graft site.
Action Tip: If you notice any of these signs, contact your oral surgeon or dentist promptly to prevent the infection from progressing.
What Causes Bacterial Infections In Bone Grafts?
Causes of Bacterial Infections in Bone Grafts
Several factors can allow bacteria to enter the graft site and cause infection, including:
- Oral bacteria entering the surgical site if proper hygiene or wound care is not maintained.
- Failure to follow post-operative instructions, such as skipping prescribed mouth rinses or not keeping the area clean.
- Wound dehiscence (opening), which exposes the graft to bacteria.
- Underlying health conditions like uncontrolled diabetes, immune disorders, or smoking, which reduce the body’s ability to fight infection.
- Rare surgical contamination, such as poor sterilization of instruments or materials.
Prevention Tip: Strict oral hygiene, careful adherence to post-op care, and regular follow-ups with your dentist or surgeon are key to lowering the risk of infection.
How Serious Are Bone Graft Infections If Left Untreated?
If left untreated, a bone graft infection can become very serious. It can lead to complete bone graft failure, requiring the removal of the grafted material and a new procedure. In severe cases, the infection can spread to other parts of the jawbone or even into the bloodstream, leading to a systemic infection (sepsis) which is a medical emergency. This is why it’s so critical to contact your surgeon immediately if you suspect an infection. For patients with insufficient jawbone, bone grafts for implants provide a strong foundation for restorations
What Long-Term Complications Can Develop From Bone Grafting?
- Bone graft failure – when the graft does not integrate with the natural bone due to poor blood supply, infection, or rejection.
- Graft resorption – gradual breakdown or shrinking of the grafted bone over time, reducing bone volume.
- Implant failure (if a dental implant is placed later) – caused by insufficient bone integration or loss of grafted bone.
- Chronic infection – a persistent low-grade infection that may remain hidden but compromise graft stability.
- Nerve damage – rare but possible if the graft area is near major nerves, leading to long-term numbness or tingling.
- Sinus complications (for upper jaw grafts) – such as sinus infections or chronic sinus issues if the graft extends into the sinus cavity.
What Is Bone Graft Rejection And How Does It Occur?
Bone graft rejection is a serious and feared complication, but it is extremely rare, especially with modern grafting materials. Rejection is when the body’s immune system recognizes the grafted material as a foreign invader and attacks it, preventing it from integrating with the existing bone. This is most often associated with allogenic (cadaver bone) or xenogeneic (animal bone) grafts, as the body can react to proteins in the donor material.
What Are The Warning Signs Of Graft Rejection?
Bone graft rejection can appear as ongoing pain, swelling, redness, or tenderness that lasts beyond the normal healing period. The graft may feel loose, exposed, or fail to integrate with the surrounding bone. Unlike an infection, these symptoms will not improve with antibiotics and often require graft removal.
How Often Does The Body Reject Bone Grafts?
Bone graft rejection is extremely rare because modern allografts and xenografts are processed to remove immune-triggering cells. Autografts, which use your own bone, have virtually zero risk of rejection. This makes graft failure due to rejection an uncommon concern in dental and surgical procedures.
Can Allergic Reactions Cause Bone Graft Failure?
Allergic reactions to bone graft materials are very uncommon since most grafts are treated to eliminate proteins that might cause sensitivity. In rare cases, patients may react to other components such as barrier membranes or fixation materials. Such reactions can lead to inflammation and swelling, which may compromise graft stability.
Wondering about the timeline? Discover how long you should wait for a dental implant after bone grafting
What Factors Lead To Bone Graft Failure?
Bone graft failure is the most common long-term risk, and it can be caused by a combination of factors. The most significant of these is poor blood supply to the graft site, which is essential for the new bone to grow and integrate. Other factors include the patient’s overall health, certain medications, and poor post-operative care. Understanding what can cause a bone graft to fail is key to avoiding this outcome.
How Does Poor Blood Supply Affect Graft Success?
Poor blood supply is one of the main culprits behind bone graft failure. The new bone material, whether from a donor or your own body, needs a rich blood supply to deliver the oxygen and nutrients necessary for cell growth and integration. If the blood supply is insufficient, the graft will not be able to “take,” and the new bone will not form, leading to a failed dental bone graft. This is a primary risk of bone grafting.
What Role Does Patient Age Play In Graft Failure?
Patient age can play a significant role in bone graft failure. While age itself doesn’t prevent a successful graft, older patients often have a slower healing process and a greater chance of having underlying medical conditions like diabetes, osteoporosis, or cardiovascular disease, all of which can affect bone healing. Therefore, a comprehensive health check is essential for older patients considering bone grafts. We use various types of bone grafts , including autografts and allografts, to rebuild bone density
Can Smoking Significantly Impact Bone Graft Success Rates?
Yes, smoking has a profound and negative impact on bone graft success rates. What Effect Does Smoking Have on Bone Grafts? The nicotine and carbon monoxide in tobacco smoke restrict blood flow and oxygen to the surgical site, significantly hindering the body’s ability to heal and integrate the new bone. Smokers have a much higher rate of graft failure, and many surgeons will refuse to perform the procedure on a patient who will not quit smoking for a period before and after the surgery.
What Are The Risks Of Incomplete Bone Integration?
Even if a bone graft doesn’t outright fail, incomplete bone integration can still be a significant risk of bone grafts for dental implants. This means that while the graft may not be rejected, it doesn’t fully fuse with the native bone, leading to a weaker foundation than desired for the final dental implant. This can result in implant instability and the need for future corrective procedures.
How Long Should Complete Integration Take?
Complete integration of a bone graft, a process known as osseointegration, typically takes a period of 4 to 9 months, though this can vary depending on the type of graft and the individual patient’s healing rate. During this time, the body’s natural bone cells grow into and around the graft material, transforming it into new, living bone. Rushing the process can lead to a significant bone graft problem.
What Happens When Bone Grafts Don’t Integrate Properly?
When bone grafts don’t integrate properly, the bone may be too soft or weak to support a dental implant. This can lead to the implant not taking hold, becoming loose, or even failing completely. This is a primary reason why surgeons wait for several months before placing the dental implant. The potential risks of receiving a bone graft that doesn’t integrate properly can mean additional surgery and cost.
Can Poor Oral Hygiene Affect Bone Integration?
Absolutely. Poor oral hygiene is one of the leading preventable causes of bone graft complications and failure. Bacteria from plaque and food debris can easily get into the surgical site, leading to an infection that compromises the graft. This is a common sign of failed dental bone graft and can completely destroy the new bone before it has a chance to heal.
What Specific Risks Are Associated With Different Types Of Bone Grafts?
The type of bone graft material used also plays a significant role in the specific risks and outcomes. The most common types are autologous, allogenic, and synthetic. Each has its own set of pros and cons, which can influence the choice of graft material for a specific procedure. A clear understanding of the risks associated with each type is essential for both the surgeon and the patient.
What Are The Risks Of Autologous Bone Grafts?
Autologous bone grafts, where bone is taken from the patient’s own body, are considered the gold standard because they carry the lowest risk of rejection. However, the procedure carries its own unique set of risks, primarily related to the secondary surgical site from which the bone is harvested.
What Complications Can Occur At The Donor Site?
The primary complications of autologous bone grafts occur at the donor site, which is often the chin, hip, or tibia. These can include pain, infection, nerve damage, and an increased risk of fracture if a large amount of bone is taken. The donor site can also be a source of significant post-operative pain and a longer recovery period. It is vital to avoid smoking after surgery , as it significantly impedes healing and can lead to complications
How Painful Is The Donor Site Recovery Process?
The donor site recovery process can often be more painful than the dental graft itself. The pain level varies depending on where the bone was harvested. Hip donor sites, for example, are known to be quite painful and can limit mobility for a few days to a week. This is a key part of the Cadaver bone grafting pros and cons debate, as cadaver grafts eliminate the need for a second surgical site.
What Are The Limitations Of Using Patient’s Own Bone?
One of the main limitations of using a patient’s own bone is the limited quantity of available bone. This makes it difficult to use for larger graft procedures. The second limitation is the need for an additional surgery, which comes with its own set of risks and a more complex recovery process. The potential risks of receiving a bone graft from yourself must be weighed against its high success rate.
What Risks Come With Allogenic Bone Grafts?
Allogenic bone grafts, which use bone from a deceased donor, are very common in bone graft procedures. While they eliminate the need for a second surgical site, they do carry a set of risks that are different from autologous grafts.
What Is The Risk Of Disease Transmission From Donor Tissue?
The risk of disease transmission from donor tissue is extremely low, but it is not zero. Donor tissue is rigorously screened and sterilized to kill any potential pathogens, including viruses like HIV and hepatitis. While the chance of a serious infection is almost negligible, it’s a risk that is still a part of the conversation. Terrified of getting a bone graft? This is an understandable concern.
How Are Allogenic Grafts Screened For Safety?
Allogenic grafts are screened for safety through a strict process that includes donor health history review, blood testing for infectious diseases, and tissue processing to remove all cells that could carry disease or trigger an immune response. This multi-layered approach makes the tissue very safe and is a primary reason why bone grafts are safe.
Can Patients Develop Immune Reactions To Donor Bone?
As mentioned earlier, immune reactions to allogenic bone grafts are extremely rare. The bone is processed to remove all cellular and protein matter that would be recognized by the body’s immune system. However, in some isolated cases, a reaction can occur, leading to a bone graft problem or failure. Cadaver bone graft rejection symptoms are very rare.
Plan your treatment effectively by learning about the comprehensive cost of bone grafting procedures
What Are The Potential Issues With Synthetic Bone Grafts?
Synthetic bone grafts, made from materials like calcium phosphate or ceramic, offer a good alternative to autografts and allografts. They eliminate the risks associated with a second surgical site and the remote risks of disease transmission. However, they are not without their own potential issues.
How Do Synthetic Materials Compare To Natural Bone?
Synthetic materials are designed to mimic the properties of natural bone, but they are not the same. They act as a scaffold for the body’s natural bone to grow into, but they don’t contain the living cells and growth factors that are present in autografts. This can sometimes lead to a slower and less predictable integration process.
What Are The Long-Term Effects Of Synthetic Bone Substitutes?
The long-term effects of synthetic bone substitutes are still being studied, but they are generally considered to be safe. Some materials are designed to be resorbed by the body as new bone grows, while others are designed to remain permanently. There is a risk that the material may not be fully resorbed or may not integrate as well as a natural bone.
Can Synthetic Grafts Cause Foreign Body Reactions?
Yes, in some rare cases, synthetic grafts can cause a foreign body reaction. This is when the body’s immune system detects the synthetic material and tries to wall it off or remove it, leading to inflammation and incomplete integration. This is a potential risk of bone grafting to consider, but it is infrequent.
How Do Medical Conditions Increase Bone Grafting Risks?
A patient’s overall health and pre-existing medical conditions can have a major impact on the success of a bone graft. Certain conditions can slow the healing process, increase the risk of infection, and compromise the body’s ability to integrate the new bone. It’s crucial for patients to be upfront about their health history.
How Does Diabetes Affect Bone Grafting Success Rates?
Diabetes is one of the most significant medical conditions that can affect bone grafting success rates. Uncontrolled blood sugar levels can impair the body’s ability to heal and fight off infection, significantly increasing the risks of bone grafting. If you experience a dental emergency, do not hesitate to contact our emergency team immediately
What Special Precautions Are Needed For Diabetic Patients?
Diabetic patients need to be monitored more closely before and after surgery. They may need to adjust their insulin or medication dosage to ensure their blood sugar is well-controlled. They are also more susceptible to infection, so a course of antibiotics may be prescribed as a preventative measure.
How Does Blood Sugar Control Impact Healing?
Blood sugar control is critical for healing. High blood sugar levels can damage blood vessels, reducing blood flow to the surgical site and hindering the delivery of essential nutrients and oxygen. It can also impair the function of white blood cells, making the body less effective at fighting off infection. This can lead to a failed dental bone graft.
What Are The Increased Infection Risks For Diabetics?
Diabetics face a significantly increased risk of infection after any surgical procedure, including bone grafting. High blood sugar creates an environment that is ideal for bacterial growth and makes the body less capable of fighting off invaders.
What Risks Do Patients With Autoimmune Diseases Face?
Patients with autoimmune diseases, such as rheumatoid arthritis or lupus, face unique risks with bone grafting. The disease itself can affect bone health and healing, and the medications used to manage these conditions can also be a factor.
How Do Autoimmune Medications Affect Bone Healing?
Many medications used to treat autoimmune diseases, particularly corticosteroids and immunosuppressants, can significantly slow down or impair the body’s natural bone healing process. This can lead to a longer recovery period and an increased risk of bone graft failure.
What Additional Monitoring Is Required For These Patients?
Patients with autoimmune diseases require additional monitoring to ensure the bone graft is healing properly. This can include more frequent follow-up visits, blood tests to check for signs of inflammation, and imaging studies to assess the graft’s integration.
Can Immunosuppressive Drugs Increase Graft Failure Rates?
Yes, immunosuppressive drugs can increase graft failure rates. By suppressing the immune system, they can prevent the body from initiating the necessary inflammatory and healing responses needed for successful bone integration.
How Do Blood Disorders Impact Bone Grafting Safety?
Blood disorders can also pose a significant risk during bone grafting procedures, primarily related to the body’s ability to clot and control bleeding. Patients on blood thinners are also at a higher risk for excessive bleeding.
What Bleeding Risks Exist For Patients On Blood Thinners?
For patients on blood thinners, the primary risk is excessive bleeding during and after the procedure. It is crucial for these patients to consult with their primary care physician to determine if it is safe to temporarily stop their medication before surgery.
How Are Clotting Disorders Managed During Surgery?
Patients with clotting disorders, such as hemophilia, require special management during surgery. This can include a team approach with a hematologist to administer clotting factors or other therapies to ensure a safe procedure.
What Pre-Operative Blood Tests Are Essential?
Essential pre-operative blood tests include a complete blood count (CBC) to check for anemia and a platelet count. For patients with a history of bleeding or on blood thinners, a coagulation panel is crucial to assess their blood’s clotting ability.
Explore your options by reading about the most effective alternatives to traditional dental implants
What Are The Risks Related To Bone Grafting Techniques And Procedures?
The risks of bone grafting can vary depending on the technique and type of graft used. Autografts (using your own bone) carry a risk of pain, infection, or nerve injury at the donor site. Allografts and xenografts have a very low risk of immune reaction or disease transmission, though these are extremely rare due to modern processing. Additionally, complex grafting procedures may increase the chance of graft failure, delayed healing, or damage to surrounding structures.
What Complications Can Arise From Sinus Lift Procedures?
- Sinus membrane perforation – the most common risk, where the thin sinus lining tears during surgery.
- Sinus infection (sinusitis) – bacteria can enter the sinus cavity, leading to inflammation or infection after the procedure.
- Graft failure – the bone graft may not integrate properly with the existing bone.
- Excessive bleeding – bleeding during or after surgery can occur, especially if blood vessels are disturbed.
- Swelling and discomfort – prolonged swelling, bruising, or pain beyond the typical healing period.
- Graft material displacement – bone particles may shift into the sinus cavity if the membrane is not fully intact.
- Delayed healing – slower recovery due to factors such as smoking, poor oral hygiene, or underlying health conditions.
What Is Sinus Membrane Perforation And How Serious Is It?
Sinus membrane perforation is the most common complication during a sinus lift procedure. It is when the surgeon accidentally tears the delicate membrane. If a small tear occurs, it can often be repaired with a special membrane, but a large tear may require the procedure to be aborted and rescheduled after the membrane has healed.
Can Sinus Infections Develop After Bone Grafting?
Yes, sinus infections can develop after bone grafting, especially after a sinus lift. The graft material can become contaminated, leading to a sinus infection that requires antibiotics and, in some cases, surgical drainage. This is a primary risk of bone grafting in the upper jaw.
What Are The Risks Of Maxillary Sinus Complications?
- Sinus infection (sinusitis) – bacterial infection causing pain, congestion, and inflammation.
- Chronic sinusitis – long-term sinus inflammation that can affect breathing and overall sinus health.
- Bone graft material displacement – graft particles can migrate into the sinus cavity, interfering with healing.
- Sinus membrane perforation – a tear in the sinus lining that increases infection and graft failure risk.
- Implant failure – insufficient bone integration due to sinus issues can prevent successful dental implant placement.
- Difficulty breathing or nasal congestion – swelling or infection may obstruct normal airflow through the sinus passages.
What Risks Are Associated With Ridge Augmentation?
Ridge augmentation is a procedure to increase the height or width of the jawbone. The main risks are soft tissue dehiscence and membrane exposure, which can lead to a failed graft.
How Common Is Soft Tissue Dehiscence?
Soft tissue dehiscence is a significant bone graft problem that occurs when the gums or soft tissue around the graft site pull apart, exposing the bone material underneath. It is not common, but can occur if there is too much tension on the gums or if the patient doesn’t follow post-operative instructions.
What Causes Membrane Exposure During Healing?
- Gum tissue recession – the gum pulls back from the surgical site, uncovering the membrane.
- Poor flap closure – inadequate suturing or tension in the gum tissue can prevent proper coverage.
- Infection or inflammation – swelling and infection can disrupt healing and cause the membrane to become exposed.
- Excessive pressure or trauma – chewing hard foods, brushing too aggressively, or accidental injury can disturb the surgical area.
- Compromised blood supply – poor circulation in the gum tissue can delay healing and lead to tissue breakdown.
Can Ridge Augmentation Affect Adjacent Teeth?
Yes, ridge augmentation can affect adjacent teeth if not performed meticulously. There is a small risk of damage to the roots of nearby teeth or the formation of periodontal pockets, which can compromise the health of those teeth.
What Risks Are Associated With Socket Preservation Procedures?
- Infection – bacteria entering the extraction site can lead to graft contamination.
- Graft failure or poor integration – the graft material may not bond properly with the surrounding bone.
- Prolonged bleeding or swelling – excessive bleeding or inflammation can delay healing.
- Membrane exposure – the protective covering over the graft may become exposed, increasing infection risk.
- Delayed healing – smoking, poor oral hygiene, or systemic health issues can slow tissue recovery.
- Pain or discomfort – localized pain beyond the normal healing period may indicate complications.
What Complications Can Occur During Immediate Grafting?
- Infection if bacteria remain in the extraction socket.
- Graft failure due to contamination or poor site preparation.
- Inadequate graft stability if the socket is not properly cleaned or shaped.
- Prolonged bleeding or delayed healing if tissues are traumatized during surgery.
How Does Timing Affect Socket Preservation Success?
- Early grafting prevents natural bone resorption after tooth extraction.
- Delayed grafting allows bone deterioration, reducing graft effectiveness.
- Late placement may require a larger or more complex graft to achieve desired results.
- Proper timing supports better implant stability in the future.
What Are The Risks Of Delayed Graft Placement?
- Increased bone loss leading to insufficient support for dental implants.
- Greater need for extensive or multiple grafting procedures.
- Longer healing time before implant placement is possible.
- Higher risk of surgical complications due to more complex bone reconstruction.
How Can Surgical Technique Errors Increase Bone Grafting Risks?
Surgical technique errors can compromise the stability and success of a bone graft. Inaccurate cuts, poor flap design, or improper handling of tissues can lead to bleeding, infection, or graft movement. Such mistakes may also damage surrounding nerves or blood vessels, increasing pain and prolonging recovery. If the graft is not secured correctly, it may fail to integrate with the natural bone, ultimately requiring revision surgery. The skill and experience of the surgeon are therefore critical for minimizing these risks.
What Happens When Surgeons Use Improper Graft Placement?
Improper placement of the bone graft prevents proper contact between the graft material and the native bone, which is necessary for integration. This can lead to graft mobility, poor healing, and eventual graft failure. Misplacement may also create gaps that allow bacteria to enter, increasing the risk of infection. In severe cases, the graft may need to be removed and replaced. Accurate positioning is key to achieving a stable and functional outcome.
How Does Incorrect Positioning Affect Healing?
Incorrect positioning of the graft can disrupt blood supply, which is essential for bone regeneration. Without sufficient blood flow, the grafted material cannot receive the oxygen and nutrients it needs to heal and fuse with the surrounding bone. Poor contact with native bone further limits cellular migration, slowing or preventing integration. This can result in delayed healing, increased pain, and a higher likelihood of graft failure. Proper alignment ensures the best chance for successful bone growth.
What Are the Consequences of Inadequate Graft Coverage?
- Graft exposure to the oral cavity, leaving it unprotected and prone to contamination.
- Bacterial infection from saliva and food particles entering the surgical site.
- Failure of graft integration due to poor healing and compromised blood supply.
- Need for additional surgery to remove or replace the exposed graft.
- Delayed or incomplete healing, even when antibiotics are used.
- Higher risk of graft loss, reducing the chances of successful implant placement later.
Can Poor Surgical Planning Lead to Complications?
Poor surgical planning increases the risk of complications before the first incision is made. Failure to evaluate bone volume, patient health, and grafting needs can result in choosing the wrong technique or materials. This oversight may lead to unstable grafts, poor healing, or the need for additional surgeries. Inadequate planning can also increase procedure time and blood loss. Careful preoperative assessment is critical to avoid unnecessary risks and improve outcomes.
What Risks Come From Inadequate Sterilization Protocols?
- Introduction of harmful bacteria directly into the graft site during surgery.
- Severe local infection that can damage the graft and surrounding bone.
- Graft failure due to contamination and inability to heal properly.
- Systemic infection (sepsis) if bacteria spread through the bloodstream.
- Delayed healing and prolonged recovery, requiring additional surgeries or treatments.
- Increased risk of antibiotic resistance if infections are difficult to treat.
How Do Contaminated Instruments Affect Outcomes?
Contaminated instruments can carry bacteria into the surgical site, creating a direct path for infection. Even a small amount of contamination can result in graft failure and require urgent treatment. Infection caused by contaminated tools may not respond well to antibiotics, increasing the risk of bone loss or systemic illness. This can significantly delay healing and compromise future implant placement. Proper sterilization of all surgical instruments is therefore non-negotiable in bone graft procedures.
What Infections Can Result From Poor Sterile Technique?
Poor sterile technique can cause localized infections, serious bone infection (osteomyelitis), or life-threatening sepsis. These may require antibiotics, surgical drainage, or graft removal. In severe cases, infection can spread to surrounding tissues or the bloodstream, endangering overall health. Strict sterilization and careful handling of instruments are critical to prevent these complications.
How Important Is Operating Room Environment Control?
A sterile operating room prevents bacteria from contaminating the graft site. Clean air systems, sterile drapes, gowns, and masks all reduce infection risk. Even small lapses can lead to serious complications or graft failure. Consistent environmental control greatly improves healing and surgical success rates.
What Are the Risks of Inexperienced Surgeon Performance?
Inexperienced surgeons may place grafts poorly, damage tissues, or miss complications. This increases infection risk, graft failure, and healing problems. They may also struggle to manage unexpected bleeding or membrane tears during the procedure. Choosing a skilled specialist greatly reduces these dangers and ensures better long-term outcomes.
How Does Surgeon Experience Impact Complication Rates?
Experienced surgeons plan better, handle complications quickly, and have lower failure rates. Their knowledge of techniques and anatomy ensures safer, more predictable outcomes. They can adapt during surgery to unexpected issues, protecting the graft and surrounding structures. This expertise directly contributes to faster recovery and higher success rates.
What Training Should Bone Graft Surgeons Have?
Bone graft surgeons should be oral surgeons or periodontists with advanced bone graft training. Years of surgical experience and a strong success record are key for safe, effective treatment. Specialized courses in bone regeneration and implantology provide additional expertise. Patients should always verify credentials and prior case results before surgery.
How Can Patients Verify Surgeon Qualifications?
Patients can verify a surgeon’s qualifications by checking their board certifications, looking at their patient reviews and testimonials, and asking them about their experience with bone grafting. It’s okay to be scared to have a bone graft, but choosing a highly qualified surgeon can provide you with significant peace of mind.
What Age-Related Risks Should Patients Consider?
Age can slow the body’s natural healing and regeneration, which may lead to a longer recovery period after a bone graft. Older patients are also more likely to have chronic conditions that can complicate surgery and healing. Careful pre-operative evaluation and tailored treatment plans help reduce these age-related risks.
What Additional Risks Do Elderly Patients Face With Bone Grafting?
Elderly patients often experience slower blood circulation and lower bone density, which can delay graft integration. They are also more likely to be on medications such as blood thinners or steroids that interfere with bone healing. These factors make close medical monitoring essential during recovery.
How Does Age Affect Bone Healing Capacity?
As people age, the production of new bone cells decreases and bone metabolism slows down. This means the graft may take longer to fuse with the existing bone and may be at a slightly higher risk of failure. Surgeons often plan for longer healing timelines in older adults.
What Medication Interactions Are More Common In Seniors?
Many seniors take multiple prescriptions for heart disease, diabetes, or osteoporosis, which can interfere with anesthesia or healing. Blood thinners can increase bleeding, while steroids may slow bone regeneration. A thorough medication review before surgery is critical to avoid harmful interactions.
How Do Age-Related Health Conditions Impact Surgery?
Conditions such as diabetes, cardiovascular disease, or a weakened immune system raise the risk of infection and slow tissue repair. These health issues can also complicate anesthesia and post-operative care. Surgeons typically require detailed medical clearance before proceeding with a graft in older patients.
What Special Considerations Apply To Younger Patients?
Younger patients may still have developing jaws, so timing is critical to avoid disrupting natural bone growth. The surgeon must also consider how the graft will support future dental needs over decades. Early planning ensures the graft remains functional as the patient matures.
How Does Jaw Development Affect Graft Timing?
If the jaw is still growing, placing a graft too early can interfere with bone formation and tooth alignment. Surgeons often wait until key growth stages are complete or carefully plan graft placement to accommodate ongoing development. This is especially important in adolescents.
What Are The Long-Term Implications For Young Adults?
Young adults need bone grafts that will remain stable for many decades, potentially supporting future implants. Proper placement and strong integration help ensure the graft lasts a lifetime. Regular dental monitoring is recommended to maintain bone health over the years.
Can Hormonal Changes Affect Bone Graft Success?
Hormonal fluctuations during puberty or young adulthood can temporarily reduce bone density. This may slow healing or require adjustments in timing and follow-up care. Surgeons often monitor hormonal factors when planning grafts for younger patients.
What Environmental And Lifestyle Factors Increase Bone Grafting Risks?
Smoking, poor diet, heavy alcohol use, and lack of oral hygiene all increase the risk of infection and graft failure. These habits reduce blood flow and weaken the immune system. Patients are encouraged to adopt healthier lifestyles before and after surgery.
How Does Smoking Impact Bone Grafting Complications?
Smoking reduces oxygen supply to the surgical site and slows new bone formation. It also increases the risk of infection and poor graft integration. Even light smoking can significantly reduce success rates.
What Specific Chemicals In Tobacco Affect Healing?
Nicotine narrows blood vessels, limiting oxygen and nutrient delivery to the graft. Carbon monoxide replaces oxygen in the blood, depriving tissues of what they need to regenerate. Together these toxins create a poor environment for bone healing.
How Long Should Patients Quit Smoking Before Surgery?
Most surgeons recommend quitting smoking at least 2–4 weeks before the procedure to allow blood flow and oxygen levels to improve. Nicotine and other toxins can linger in the body, so an early stop gives tissues time to recover. Patients are also advised to remain smoke-free for 3–6 months after surgery to give the graft the best chance of successful integration. Even a few cigarettes during recovery can reduce oxygen supply and increase infection risk
What Are The Statistics On Smoking And Graft Failure?
Studies consistently show that smokers have double or even triple the failure rate of non-smokers when it comes to bone grafting. Nicotine restricts blood vessels, reducing the nutrients and oxygen required for bone regeneration. In some research, up to 20–30% of grafts failed in smokers, compared to less than 10% in non-smokers. Healing time is also significantly longer, increasing the chance of infection.
What Role Does Nutrition Play In Bone Grafting Risks?
Good nutrition provides the raw materials your body needs to form new bone and repair soft tissue. Diets rich in protein, calcium, vitamin D, vitamin K, and zinc help strengthen the immune system and speed recovery. Poor nutrition, on the other hand, slows cell growth and increases the risk of infection or graft failure. Surgeons often recommend starting a nutrient-rich eating plan several weeks before surgery. Drinking enough water is equally important, as dehydration can reduce blood circulation to the graft site.
How Do Vitamin Deficiencies Affect Bone Healing?
Vitamin D is critical for calcium absorption, while vitamin K supports proper bone mineralization. Deficiencies in these or other nutrients such as calcium and magnesium can delay healing and increase the chance of graft rejection. Low vitamin C levels also weaken collagen production, which is essential for the gum and bone structure around the graft.
What Dietary Restrictions Should Patients Follow?
Patients are usually placed on a soft-food diet for at least 1–2 weeks after surgery to prevent pressure on the graft. Foods such as yogurt, smoothies, mashed vegetables, scrambled eggs, and protein shakes are ideal during this phase. Hard, crunchy, or spicy foods can disturb the surgical site and delay healing. Alcohol and sugary drinks should also be avoided because they promote inflammation and infection. As healing progresses, the surgeon will guide when to gradually return to a normal diet.
Can Malnutrition Lead To Graft Complications?
Yes, malnutrition is a serious risk factor for graft failure. A body lacking essential vitamins, proteins, or calories cannot build new bone efficiently or fight infection. Patients who are underweight, recovering from illness, or following restrictive diets are particularly vulnerable. Surgeons may recommend protein shakes or specific supplements before and after surgery. Addressing malnutrition early helps ensure proper graft integration and long-term stability.
How Do Alcohol And Drug Use Affect Bone Grafting Safety?
Both alcohol and recreational drugs interfere with the body’s natural healing processes. Alcohol can thin the blood, increase bleeding during surgery, and weaken the immune system, while drugs such as cocaine or marijuana can reduce blood flow to the graft site. These substances also interact with anesthesia and prescription medications, increasing surgical risks.
What Are The Risks Of Alcohol Consumption Before Surgery?
Drinking alcohol in the days leading up to surgery increases the chance of excessive bleeding and slower clot formation. Alcohol also dehydrates the body, making it harder to maintain proper blood pressure during anesthesia. After surgery, alcohol can interfere with prescribed painkillers or antibiotics, reducing their effectiveness. Most surgeons recommend avoiding alcohol for at least one week before and two weeks after the procedure. Long-term heavy drinkers may require additional medical clearance.
How Do Recreational Drugs Impact Healing?
Recreational drugs such as cannabis, cocaine, and amphetamines can significantly delay healing by restricting blood flow or suppressing immune responses. Some drugs may also interact dangerously with anesthesia, increasing the risk of cardiac or respiratory complications during surgery. Patients who use these substances may experience longer recovery times and higher infection rates.
What Medication Interactions Should Patients Avoid?
Certain medications can thin the blood or interfere with bone healing. Aspirin, ibuprofen, blood thinners (like warfarin), and some herbal supplements such as ginkgo or garlic should often be paused before surgery. Steroids and osteoporosis medications may also slow bone regeneration. Always follow your surgeon’s instructions before stopping or adjusting any medication.
What Are The Financial And Psychological Risks Of Bone Grafting?
Bone grafting can be physically and emotionally demanding while also carrying significant financial costs. Complications may require extra treatments that insurance does not fully cover. Patients may experience anxiety about the outcome, frustration with long recovery periods, or fear of additional procedures. Financial stress, combined with the physical discomfort of surgery, can affect overall well-being. Careful planning and mental health support are key to managing these risks.
What Financial Risks Should Patients Consider?
Bone grafting is often an out-of-pocket expense, particularly if it is performed for dental implants rather than medical necessity. Costs can range from a few hundred to several thousand dollars depending on the graft type, anesthesia, and location. If complications arise, follow-up surgeries, imaging scans, and medications add to the total bill.
What Happens If Additional Procedures Are Needed?
If the graft fails or does not integrate, revision surgery may be required to replace or rebuild the bone. These follow-up procedures are typically more complex and can extend the recovery timeline by several months. Surgeons may use alternative graft materials or add growth factors to encourage healing. Each additional surgery increases overall costs and may involve new risks, such as infection or nerve damage.
How Much Do Complication Treatments Typically Cost?
The cost of managing complications varies depending on severity. Minor infections might only require antibiotics costing a few hundred dollars, while a failed graft needing revision can cost several thousand dollars. Hospital stays, advanced imaging, and anesthesia can raise costs further. Patients should maintain an emergency fund or payment plan to reduce financial stress if complications occur.
What Insurance Coverage Exists For Failed Grafts?
Many insurance plans cover initial grafting but may limit or exclude coverage for repeat procedures. Some policies also separate anesthesia and hospital fees, which might not be reimbursed fully. Patients should request a written explanation of benefits and submit a pre-authorization to confirm what is included. Reviewing coverage early prevents surprise bills and helps plan for possible out-of-pocket expenses.
What Psychological Risks Are Associated With Bone Grafting?
Anxiety, fear of pain, and uncertainty about the outcome are common emotional challenges. Extended healing periods can lead to frustration, mood swings, or even depression. Some patients develop dental phobia after a difficult graft experience, making future treatments stressful. Seeking professional counseling or joining a support group can provide valuable coping strategies.
How Do Patients Cope With Extended Treatment Times?
Recovery can take three to six months or longer, which requires patience and emotional resilience. Setting small milestones, such as tracking pain reduction or improved diet, can help maintain motivation. Many patients benefit from mindfulness practices, gentle exercise, or professional therapy. Staying in regular contact with the surgical team provides reassurance and guidance throughout the process.
What Mental Health Support Is Available During Recovery?
Patients can access support through therapists, mental health counselors, or online dental recovery communities. Some dental clinics also provide patient coordinators who help monitor emotional well-being. Video counseling sessions are available for those who prefer privacy or cannot attend in-person appointments. Early mental health care can prevent anxiety from becoming overwhelming.
How Common Is Anxiety About Bone Graft Procedures?
Anxiety is extremely common, especially for patients undergoing dental surgery for the first time. Fear of pain, complications, or implant failure can be overwhelming. Learning about the procedure, asking questions, and working with an experienced surgeon helps reduce worry. In some cases, sedation or relaxation medications may be recommended to keep patients calm.
What Pre-Operative Steps Reduce Bone Grafting Complications?
Comprehensive pre-operative planning is key to reducing risks. Surgeons often recommend blood tests, dental cleanings, and imaging scans to assess bone quality. Patients may also be advised to quit smoking, improve nutrition, and manage chronic conditions before surgery. These steps ensure the body is in the best possible condition for healing.
What Medical Evaluations Are Essential Before Surgery?
Blood tests check for infection, vitamin deficiencies, and clotting issues. X-rays or CT scans evaluate bone density and the exact grafting site. A review of heart and lung health ensures the patient can safely undergo anesthesia. Any abnormal results may lead to adjustments in the surgical plan or temporary delays for treatment.
How Should Patients Prepare Their Immune System?
Eating a diet rich in fruits, vegetables, and lean proteins strengthens the immune system and promotes bone healing. Adequate sleep, stress management, and proper hydration are equally important. Patients with chronic illnesses such as diabetes should work with their doctor to achieve stable blood sugar levels before surgery. Some surgeons may recommend vitamin or mineral supplements if deficiencies are detected.
What Medications Should Be Stopped Before Surgery?
Blood thinners, certain anti-inflammatory drugs, and herbal supplements like ginseng or fish oil may need to be paused. These substances increase bleeding risks and can complicate anesthesia. Patients should never stop medications on their own; all changes must be supervised by the surgeon or prescribing doctor. A personalized schedule will be provided to ensure safe timing.
What Post-Operative Care Minimizes Risk Of Complications?
Strict oral hygiene, prescribed mouth rinses, and a soft-food diet are essential after surgery. Patients should avoid smoking, alcohol, and strenuous activities for several weeks. Follow-up visits allow early detection of infection or poor graft integration. Sleeping with the head elevated and using ice packs can reduce swelling and discomfort.
How Should Patients Manage Pain And Swelling?
Pain and swelling are normal during the first few days but can be managed with ice packs, prescription painkillers, and over-the-counter anti-inflammatories (if approved by the surgeon). Elevating the head during rest helps fluid drain and reduces swelling. Any sudden increase in pain or bleeding should be reported immediately. Gentle saline rinses may also soothe the surgical site without disturbing the graft.
What Signs Require Immediate Medical Attention?
High fever, severe or worsening pain, persistent bleeding, or pus around the graft site are warning signs of infection. Numbness, difficulty breathing, or uncontrolled swelling also require urgent evaluation. Prompt treatment can prevent graft failure and reduce the need for revision surgery.
How Long Should Patients Follow Dietary Restrictions?
Most patients follow a soft diet for 1–2 weeks, but large or complex grafts may require longer. Foods should be easy to chew and nutrient-rich to support healing. Gradual reintroduction of harder foods should only occur once the surgeon confirms sufficient bone stability. Chewing on the opposite side of the mouth protects the graft during early recovery.
What Role Does Follow-Up Care Play In Risk Reduction?
Regular follow-up visits are essential to monitor healing, detect infection, and ensure proper graft integration. These appointments allow the surgeon to adjust medications or recommend additional imaging if needed. Early intervention during these visits can prevent small issues from becoming serious complications.
How Often Should Patients Visit For Post-Op Checkups?
Initial checkups typically occur within 3–7 days after surgery, followed by visits at two weeks, one month, and several months post-op. More complex cases may require extra imaging and closer monitoring. Patients with chronic health conditions may also be scheduled for more frequent evaluations.
What Imaging Studies Monitor Graft Success?
Dental X-rays, panoramic images, and CT scans show how well the graft is bonding with the natural bone. Advanced 3D imaging can detect small changes in bone density and growth over time. These studies help the surgeon decide when it is safe to proceed with implants or additional treatments.
When Can Patients Resume Normal Activities Safely?
Most patients can resume light activities like walking or desk work within 1–2 days, but strenuous exercise or heavy lifting should wait 2–4 weeks. Chewing hard foods or using the graft site is usually avoided for 4–6 weeks or until the surgeon confirms healing. Recovery time may be longer for smokers or patients with health issues, so always follow your surgeon’s specific instructions.
[sc_fs_multi_faq headline-0=”h3″ question-0=”What is the most serious risk of bone grafting?” answer-0=”Severe infection or total graft failure is the most serious risk, which can lead to graft removal and repeat surgery.” image-0=”” headline-1=”h3″ question-1=”How often do bone graft infections occur?” answer-1=”Infections are uncommon, affecting roughly 1–5% of cases when proper sterilization and aftercare are followed.” image-1=”” headline-2=”h3″ question-2=”Can bone grafts cause cancer?” answer-2=”No, bone grafts do not cause cancer; the materials used are biocompatible and well-studied.” image-2=”” headline-3=”h3″ question-3=”What happens if my body rejects the bone graft?” answer-3=”Rejection is rare but may cause pain, swelling, and graft failure, requiring removal or revision.” image-3=”” headline-4=”h3″ question-4=”Is bone grafting more risky for smokers?” answer-4=”Yes, smoking reduces blood flow and doubles the risk of infection, delayed healing, and graft failure.” image-4=”” headline-5=”h3″ question-5=”How long do bone grafting risks last?” answer-5=”Most risks are highest in the first 2–6 weeks, though full integration takes several months.” image-5=”” headline-6=”h3″ question-6=”Can I prevent bone graft complications?” answer-6=”Yes—quit smoking, follow aftercare instructions, eat a healthy diet, and attend all follow-up visits.” image-6=”” headline-7=”h3″ question-7=”What are the warning signs of bone graft failure?” answer-7=”Persistent pain, swelling, bleeding, pus, or loose implants are key warning signs.” image-7=”” headline-8=”h3″ question-8=”Is bone grafting safe for elderly patients?” answer-8=”Yes, if overall health is stable and medical conditions are well managed.” image-8=”” headline-9=”h3″ question-9=”What should I do if I experience severe pain after bone grafting?” answer-9=”Contact your surgeon immediately to rule out infection or other complications” image-9=”” headline-10=”h3″ question-10=”Can bone grafts affect my ability to taste food?” answer-10=”Temporary taste changes can occur but usually resolve within weeks.” image-10=”” headline-11=”h3″ question-11=”How do I know if my bone graft is healing properly?” answer-11=”Stable gums, decreasing pain, and normal X-ray results at follow-ups indicate good healing.” image-11=”” headline-12=”h3″ question-12=”What medications increase bone grafting risks?” answer-12=”Blood thinners, steroids, and osteoporosis drugs (like bisphosphonates) can delay healing or increase bleeding.” image-12=”” headline-13=”h3″ question-13=”Can stress affect bone graft healing?” answer-13=”Yes, stress weakens immunity and slows healing by affecting blood flow and hormone levels.” image-13=”” headline-14=”h3″ question-14=”Are there alternatives to bone grafting with fewer risks?” answer-14=”Yes—options include sinus lifts, ridge expansion, or short dental implants depending on bone quality.” image-14=”” headline-15=”h3″ question-15=”How common are nerve complications from bone grafts?” answer-15=”Nerve issues are rare, occurring in less than 1% of cases, and are usually temporary.” image-15=”” headline-16=”h3″ question-16=”Can bone grafts cause sinus problems?” answer-16=”Only upper jaw grafts near the sinuses carry a small risk of sinus infection or pressure.” image-16=”” headline-17=”h3″ question-17=”What happens if I get pregnant after bone grafting?” answer-17=”Once healing begins, pregnancy is generally safe, but inform your dentist and obstetrician.” image-17=”” headline-18=”h3″ question-18=”How do I choose a qualified bone graft surgeon?” answer-18=”Look for a board-certified oral surgeon or periodontist with extensive grafting experience and strong patient reviews.” image-18=”” headline-19=”h3″ question-19=”What questions should I ask my dentist about bone grafting risks?” answer-19=”Ask about their experience, infection rates, healing time, graft materials, and emergency procedures.” image-19=”” count=”20″ html=”true” css_class=””]